Optimal thermal environment during infant sleep is critical for ensuring restful and safe slumber. Maintaining an appropriate room climate, coupled with suitable bedding and clothing, supports the regulation of the infant’s core body warmth. Factors influencing this include ambient conditions and the child’s physiological state.
Proper management of the child’s surroundings during sleep contributes to decreased risk of overheating, a significant factor associated with Sudden Infant Death Syndrome (SIDS). Furthermore, conducive conditions can improve sleep quality, promoting healthy development and growth. Historically, emphasis on these considerations has evolved alongside advancements in pediatric medicine and awareness of infant safety.
The subsequent discussion will delve into practical guidelines for creating a thermally balanced sleep environment for infants, covering topics such as room thermostat settings, appropriate clothing choices, and recognizing signs of overheating or being too cold.
Guidance for Establishing Optimal Infant Sleep Climates
This section outlines actionable recommendations for caregivers aiming to cultivate a thermally appropriate sleep environment for infants. Attention to these details promotes both safety and restful slumber.
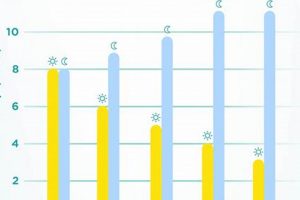
Tip 1: Maintain a Consistent Room Temperature: A thermostat setting between 68-72 degrees Fahrenheit (20-22 degrees Celsius) is generally recommended. This range supports the infant’s thermoregulation during sleep.
Tip 2: Choose Lightweight Bedding: Avoid heavy blankets, quilts, or comforters. Opt for lightweight, breathable materials like cotton or muslin to minimize the risk of overheating.
Tip 3: Dress the Infant Appropriately: Consider a single layer of breathable clothing, such as a cotton onesie or sleep sack. Avoid overdressing, which can lead to increased body warmth.
Tip 4: Monitor for Signs of Overheating: Indicators may include flushed skin, rapid breathing, sweating, or restlessness. Promptly adjust the environment or the infant’s clothing if these signs are observed.
Tip 5: Consider a Fan for Air Circulation: A small fan can improve air circulation in the room, aiding in temperature regulation and potentially reducing the risk of SIDS. Ensure the fan is not directed directly at the infant.
Tip 6: Ensure Proper Ventilation: Proper ventilation in the room assists in air circulation. Open a window slightly or ensure the HVAC system is working correctly.
Tip 7: Utilize Sleep Sacks or Wearable Blankets: These provide warmth without the dangers associated with loose bedding. Ensure the sleep sack is sized appropriately for the infant’s weight and height.
Implementing these guidelines minimizes the risk of overheating and enhances the infant’s comfort during sleep. Observation and adjustments are crucial to maintain a safe and restful environment.
The concluding section will synthesize these recommendations and address potential complications that may arise in maintaining an ideal infant sleep environment.
1. Room Thermostat Setting
The room thermostat setting is a foundational element in managing an infant’s thermal environment during sleep. As infants possess a limited capacity for independent thermoregulation, the ambient temperature of their sleep space directly influences their core body warmth. A thermostat setting that is too high increases the risk of overheating, a factor implicated in Sudden Infant Death Syndrome (SIDS). Conversely, a setting that is too low can lead to hypothermia, potentially compromising the infant’s physiological stability. Studies by pediatric health organizations consistently emphasize maintaining a consistent, moderate room temperature as a key component of safe infant sleep practices.
Practical application of this principle involves diligent monitoring of the room’s temperature using a reliable thermometer, coupled with appropriate adjustments to the thermostat. For example, during winter months, supplemental heating may be necessary to maintain the recommended temperature range of 68-72 degrees Fahrenheit (20-22 degrees Celsius). Conversely, in warmer months, air conditioning or fans may be required to prevent overheating. Caregivers should also be mindful of external factors that may influence the room temperature, such as direct sunlight exposure or drafts. Regular assessment and adaptation are vital for ensuring the infant’s thermal comfort and safety.
In summary, the room thermostat setting is a critical and controllable variable that directly impacts infant sleep warmth. Challenges arise from inconsistent monitoring, seasonal variations, and inaccurate thermostat readings. Prioritizing accurate temperature maintenance, through the use of reliable tools and consistent monitoring, is a primary responsibility of caregivers in promoting safe sleep practices and overall infant well-being. This contributes significantly to mitigating risks associated with imbalanced thermoregulation during sleep.
2. Appropriate Clothing Layers
The selection of appropriate clothing layers for an infant is intrinsically linked to the maintenance of optimal thermal conditions during sleep. Overdressing increases the risk of overheating, whereas insufficient clothing may lead to hypothermia, both of which compromise infant well-being. Proper layering seeks to balance warmth and breathability, facilitating the regulation of core body warmth within a safe and comfortable range. For example, a single layer of breathable cotton clothing might suffice in a room maintained at the recommended temperature. Conversely, in a slightly cooler environment, a lightweight sleep sack or wearable blanket may be necessary to provide additional insulation without the hazards associated with loose bedding.
The practical significance of understanding the impact of clothing layers on infant thermoregulation extends to daily routines and seasonal adjustments. Parents and caregivers must adapt clothing choices based on ambient conditions, factoring in both the room temperature and the infant’s individual characteristics. Infants display varying metabolic rates, influencing their capacity to generate and retain body warmth. Therefore, monitoring the infant for signs of overheating (e.g., flushed skin, sweating, rapid breathing) or being too cold (e.g., shivering, cool extremities) becomes a crucial component of responsible caregiving. Furthermore, understanding the properties of different fabrics, such as the breathability of cotton versus the insulating properties of fleece, enables informed decision-making when selecting appropriate sleepwear.
In summary, the selection of appropriate clothing layers represents a modifiable variable in maintaining optimal warmth during infant sleep. Vigilant observation of the infant’s physiological cues, awareness of environmental factors, and informed material choices contribute to minimizing the risks of thermal imbalance. The challenge lies in tailoring clothing choices to individual needs and fluctuating conditions. By embracing this knowledge, caregivers can actively promote a safe and restful sleep environment for infants, directly supporting their health and development.
3. Bedding Material Choice
The selection of bedding material exerts a direct influence on an infant’s thermal regulation during sleep. The composition and properties of the fabric impact heat retention, breathability, and moisture wicking, each of which contribute to the overall warmth of the sleep environment.
- Fiber Composition and Breathability
Natural fibers, such as cotton and muslin, exhibit enhanced breathability compared to synthetic alternatives. This characteristic facilitates air circulation, preventing the accumulation of excess warmth and minimizing the risk of overheating. Conversely, materials with limited breathability, such as fleece or certain synthetic blends, may trap heat, leading to discomfort and potential health risks.
- Heat Retention Properties
Different materials possess varying capacities for retaining warmth. While some degree of heat retention is necessary to maintain a comfortable sleep temperature, excessive retention can be detrimental. For example, a thick down comforter, while suitable for older children or adults, poses a significant overheating risk for infants due to its high insulating properties. Bedding options should prioritize moderate insulation balanced with breathability.
- Moisture Wicking Capabilities
Infants may experience perspiration during sleep, particularly in warmer environments. Materials with moisture-wicking capabilities, such as merino wool or certain synthetic performance fabrics, draw moisture away from the skin, promoting dryness and preventing discomfort. The selection of moisture-wicking bedding can contribute to maintaining a stable and comfortable warmth level throughout the night.
- Allergenic Potential
The allergenic potential of bedding materials also influences the selection process. Certain fabrics may harbor dust mites or trigger allergic reactions in sensitive infants, potentially disrupting sleep and affecting overall health. Hypoallergenic materials, such as bamboo or tightly woven cotton, can minimize the risk of allergic reactions and contribute to a more restful sleep environment.
In conclusion, the choice of bedding material represents a crucial aspect of managing the sleeping environment. Prioritizing breathable, moderately insulating, moisture-wicking, and hypoallergenic fabrics promotes optimal thermal regulation and minimizes potential health risks. Considerations of the infant’s individual needs, environmental conditions, and material properties facilitate informed decision-making and contribute to safe sleep practices.
4. Air Circulation Importance
Effective air circulation plays a critical role in maintaining optimal warmth during infant sleep. Stagnant air can lead to localized heat buildup around the infant, elevating the risk of overheating. This risk is compounded in environments with poor ventilation or inadequate airflow. Air circulation facilitates the dissipation of excess heat, promoting a more uniform and stable warmth across the sleep environment. The absence of adequate circulation disrupts thermoregulation, potentially triggering physiological stress responses in the infant.
The practical application of this principle involves the strategic use of fans or ventilation systems to ensure consistent airflow throughout the infant’s sleep space. For instance, a small, oscillating fan placed at a distance from the crib can effectively circulate air without directly exposing the infant to a draft. Similarly, ensuring that heating and cooling systems are functioning optimally contributes to consistent air movement. Caregivers must also avoid obstructing ventilation pathways with furniture or bedding, thereby minimizing the potential for localized heat accumulation. Real-life examples illustrating the impact of air circulation include instances where infants sleeping in poorly ventilated rooms experience elevated body temperatures, prompting interventions such as opening windows or adding a fan.
In conclusion, the importance of air circulation as a component of maintaining appropriate warmth during infant sleep cannot be overstated. It directly influences thermoregulation and mitigates the risk of overheating. While achieving optimal air circulation presents challenges related to balancing airflow with the avoidance of drafts, the implementation of straightforward strategies significantly enhances infant safety and well-being. Understanding and addressing the dynamics of airflow forms an integral part of responsible caregiving and promotes healthy sleep habits.
5. Overheating Risk Factors
Elevated body temperature during infant sleep poses a significant threat to health and well-being. Recognition and mitigation of these risks are critical components of creating a secure and conducive sleep environment.
- Excessive Room Warmth
Elevated ambient temperature in the sleep environment is a primary contributor to infant overheating. When the surrounding air is too warm, the infant struggles to dissipate body warmth effectively, leading to a rise in core temperature. Rooms exceeding the recommended range of 68-72F (20-22C) create a high-risk setting.
- Inappropriate Clothing Layers
Overdressing infants increases the likelihood of overheating. Multiple layers of clothing or heavy fabrics restrict the body’s ability to release heat, causing core temperature to rise. Selecting breathable, lightweight materials and avoiding excessive layering is essential.
- Heavy Bedding Materials
Thick blankets, quilts, and comforters impede heat dissipation. These materials trap warmth around the infant’s body, contributing to elevated temperature levels. Lightweight, breathable bedding, such as cotton or muslin, is preferable.
- Compromised Air Circulation
Insufficient airflow hinders heat exchange between the infant and the surrounding environment. Stagnant air allows heat to accumulate around the infant’s body, elevating the risk of overheating. Ensuring adequate ventilation or using a fan can mitigate this risk.
These factors underscore the necessity of vigilant monitoring and proactive adjustments to the infant’s sleep environment. By addressing these variables, caregivers can significantly minimize the potential for overheating and promote a safe and healthful sleep experience.
6. Hypothermia Identification
The recognition of hypothermia in infants is critically linked to maintaining optimal thermal conditions during sleep. As an infant’s thermoregulatory system is immature, its ability to generate and conserve warmth in response to a cold environment is limited. Prompt identification of hypothermia allows for timely intervention, minimizing potential health consequences associated with prolonged exposure to cold.
- Core Temperature Assessment
Accurate measurement of an infant’s core temperature is fundamental in identifying hypothermia. Rectal or axillary temperature readings below 97F (36.1C) necessitate immediate evaluation. Reliance on tactile assessment alone (e.g., feeling the infant’s extremities) is insufficient due to its subjective nature. An objective measurement provides an accurate indication of the infant’s thermal status and informs appropriate interventions.
- Behavioral Indicators
Behavioral cues may provide early indications of hypothermia, though these can be subtle and easily misinterpreted. Lethargy, decreased activity, and reluctance to feed can suggest the infant is expending energy to maintain warmth. Paradoxical irritability may also manifest. Observation of these behavioral changes, in conjunction with temperature assessment, enhances diagnostic accuracy.
- Physiological Signs
Physiological manifestations of hypothermia include cool or cold extremities, pale or mottled skin, and slowed respiratory rate. In severe cases, bradycardia (slow heart rate) may develop. Recognition of these signs demands immediate action to rewarm the infant and prevent further decline. Delayed identification can lead to severe complications, including respiratory distress and metabolic acidosis.
- Environmental Risk Factors
Assessment of the sleeping environment for potential hypothermia risk factors is paramount. These risks include a room temperature below the recommended range (68-72F or 20-22C), drafts, inadequate clothing, and the use of thin or insufficient bedding. Correction of these environmental factors is essential for preventing recurrent hypothermia episodes.
The integration of core temperature assessment, behavioral observation, physiological sign recognition, and environmental risk factor evaluation is crucial in the effective identification of hypothermia in infants. This multifaceted approach enables prompt intervention and safeguards the infant’s health and well-being within the context of maintaining proper thermal management during sleep.
7. Safe Sleep Practices
Safe sleep practices and the management of warmth during infant sleep are intrinsically linked, forming a cornerstone of infant health and well-being. Deviations from recommended safe sleep guidelines, such as the use of loose bedding or inappropriate sleep surfaces, can exacerbate the risks associated with temperature dysregulation. For instance, loose blankets can contribute to overheating, while a lack of adequate bedding in a cold environment may lead to hypothermia. The consistent implementation of safe sleep practices serves as a protective measure against adverse thermal events, directly impacting infant safety and reducing the risk of Sudden Infant Death Syndrome (SIDS).
Consider the example of an infant placed to sleep on a soft mattress with several layers of blankets in a warm room. This scenario combines multiple risk factors, increasing the likelihood of overheating and potential suffocation. Conversely, an infant sleeping on a firm, flat surface with a lightweight sleep sack in a room maintained at the appropriate temperature exemplifies a safe sleep environment that minimizes thermal risks. Practical application of these principles requires caregivers to adhere to evidence-based recommendations, including placing infants on their backs to sleep, using a firm sleep surface, avoiding loose bedding, and maintaining a moderate room temperature. Educational initiatives aimed at promoting safe sleep practices should emphasize the crucial role of proper warmth management, equipping caregivers with the knowledge and skills necessary to create a thermally safe sleep environment.
In summary, the integration of safe sleep practices and the management of warmth represents a holistic approach to infant care. Adherence to safe sleep guidelines mitigates potential thermal risks, promoting healthy sleep and reducing the incidence of adverse outcomes. Challenges arise from inconsistent adherence to recommendations, cultural practices, and misinformation. Continuous education and reinforcement of evidence-based practices are essential in ensuring that caregivers prioritize infant safety and well-being by creating a safe sleep environment.
Frequently Asked Questions
The following questions address common concerns regarding maintaining proper environmental conditions for infant sleep.
Question 1: What is the ideal room climate for infant sleep?
The generally recommended range is 68-72 degrees Fahrenheit (20-22 degrees Celsius). This range minimizes the risk of overheating and hypothermia.
Question 2: How many layers of clothing are appropriate for an infant during sleep?
A single layer of breathable clothing, such as a cotton onesie or sleep sack, is often sufficient. Overdressing should be avoided.
Question 3: Is it safe to use blankets in an infant’s crib?
Loose blankets are not recommended due to the risk of suffocation. Sleep sacks or wearable blankets provide warmth without posing a similar hazard.
Question 4: What are the signs of overheating in an infant during sleep?
Flushed skin, rapid breathing, sweating, and restlessness may indicate overheating. Prompt action to cool the infant is necessary.
Question 5: Is a fan safe for use in an infant’s room during sleep?
A fan can improve air circulation, potentially reducing the risk of SIDS. It should not be directed directly at the infant and should be placed at a safe distance.
Question 6: How often should the room temperature be checked?
The room temperature should be checked regularly, especially during seasonal changes. Adjustments to heating or cooling systems may be required to maintain the recommended range.
Maintaining appropriate conditions is a critical aspect of safe sleep practices. Vigilant monitoring and adjustments based on the infant’s individual needs are essential.
The following section will summarize the key recommendations for optimizing conditions, providing a concise overview of best practices.
Sleep Temperature Baby
This article has explored the multifaceted relationship between sleep environment warmth and infant well-being. The maintenance of appropriate ambient conditions, the careful selection of bedding and clothing, and the awareness of overheating and hypothermia risks are all critical elements. Consistent adherence to safe sleep guidelines reinforces the importance of creating a thermally balanced sleep space. The long-term health benefits derived from a stable environment underscore the significance of the preceding recommendations.
Prioritizing infant sleep environment conditions is not merely a matter of comfort but a fundamental responsibility for caregivers. Diligent monitoring, proactive adjustments, and a commitment to evidence-based practices are essential for minimizing risks and promoting healthy development. The vigilance exercised in creating an optimal sleep environment directly translates to improved infant health outcomes and a reduction in preventable adverse events.