Infant sleepwear crafted from bamboo-derived fabric is designed to provide a comfortable and safe environment for a baby’s rest. These garments, typically one-piece outfits with enclosed feet, are intended for nighttime use. Examples include footed pajamas and sleep sacks made from this soft, breathable material.
The appeal of these products stems from the inherent properties of the raw material. It is known for its exceptional softness, hypoallergenic qualities, and moisture-wicking capabilities, making it suitable for sensitive skin. Historically, natural fibers have been favored for infant apparel due to their gentle nature and ability to regulate temperature, promoting more restful sleep for babies and offering peace of mind for caregivers.
The remainder of this discussion will address the specific characteristics of sleepwear produced from this plant-based textile, including its environmental advantages, care instructions, and considerations for selecting the appropriate size and style for infants of varying ages and developmental stages.
Selection and Use Guidance
Considerations for choosing and maintaining sleepwear of this type can optimize its benefits and longevity.
Tip 1: Prioritize Fabric Composition: Verify that the material is genuinely derived from bamboo and free from harmful chemicals. Look for certifications that confirm the fabric’s safety and quality.
Tip 2: Assess Seam Construction: Examine the seams for smoothness and ensure they are flat to prevent irritation against delicate skin.
Tip 3: Select Appropriate Size: Choose a size that allows freedom of movement without being excessively loose, which could pose a safety hazard. Consult size charts and consider the infant’s weight and length.
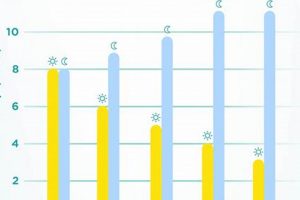
Tip 4: Monitor Room Temperature: Adjust the layering beneath the garment based on the ambient temperature to prevent overheating or chilling. A lightweight undershirt may be suitable for cooler environments.
Tip 5: Follow Care Instructions: Adhere to the manufacturer’s washing and drying recommendations to maintain the fabric’s softness and prevent shrinkage. Gentle detergents are advisable.
Tip 6: Inspect Regularly for Wear: Examine the sleepwear periodically for signs of wear and tear, such as holes or loose threads, and replace it as needed to ensure safety.
Tip 7: Consider TOG Rating for Sleep Sacks: If using a sleep sack version, choose the appropriate Thermal Overall Grade (TOG) rating based on the room temperature to maintain a comfortable and safe sleeping environment.
Adhering to these guidelines will contribute to the safe and effective utilization of infant sleepwear crafted from this material, maximizing its comfort and promoting restful sleep.
The following section will delve into the potential environmental impact of this fabric and offer suggestions for responsible disposal or recycling.
1. Softness
The tactile property of softness is a primary attribute influencing the selection of infant sleepwear. Sleepwear manufactured from bamboo-derived fabric is frequently chosen specifically for its perceived softness, which is believed to enhance comfort and minimize potential skin irritation. This inherent characteristic stems from the smooth, round structure of the plant-based fibers, contrasting with the potentially coarser texture of some synthetic or conventionally produced cotton alternatives. The causality is straightforward: smoother fibers result in a gentler contact against the skin. The importance of softness is amplified by the delicate nature of infant skin, which is more susceptible to chafing and discomfort.
Practical examples demonstrate the significance of this attribute. Infants wearing garments made from rougher materials may exhibit restlessness or skin reactions, potentially disrupting sleep patterns. Conversely, sleepwear that is perceived as soft is hypothesized to promote relaxation and improve sleep quality. Clinical experience also suggests that premature infants, particularly sensitive to tactile stimuli, may benefit from being swaddled or dressed in exceptionally soft materials. Retailers frequently highlight softness in marketing campaigns, emphasizing the experiential benefits for both the child and caregiver. This includes customer reviews and ratings frequently mentioning this as a key differentiator.
In summary, the connection between bamboo-derived infant sleepwear and the characteristic of softness is crucial for the comfort and well-being of the infant. While subjective assessment of softness can vary, the smoother fiber structure of bamboo supports the rationale for its selection in this context. Further research to empirically quantify the impact of fabric softness on infant sleep and skin health would strengthen this understanding and inform best practices in infant apparel design and selection.
2. Breathability
The characteristic of breathability is paramount in the selection of infant sleepwear, particularly regarding thermal regulation and the prevention of overheating. Sleepwear constructed from bamboo-derived fabric is often touted for its superior breathability relative to synthetic alternatives, influencing its suitability for infants.
- Fiber Structure and Air Permeability
Bamboo fibers exhibit a porous structure, facilitating increased air permeability compared to tightly woven synthetic materials. This porosity allows for improved ventilation, enabling the dissipation of heat and moisture away from the infant’s skin. The role of air permeability is direct: a higher permeability coefficient corresponds to a greater capacity for air exchange, reducing the likelihood of heat retention and subsequent discomfort. Example: infants sleeping in environments with elevated ambient temperatures are particularly vulnerable to overheating; breathable sleepwear mitigates this risk.
- Moisture Management and Evaporation
Breathability is inextricably linked to moisture management. The ability of a fabric to absorb and wick moisture away from the skin promotes evaporative cooling. Garments crafted from this material typically demonstrate superior moisture-wicking capabilities, contributing to a drier and more comfortable sleep environment. Example: nocturnal perspiration in infants can lead to chilling upon subsequent cooling; effective moisture management reduces this risk.
- Thermal Regulation and Overheating Prevention
The primary implication of breathability is its impact on thermal regulation. Infants possess a limited capacity to regulate their body temperature, rendering them susceptible to both overheating and chilling. Highly breathable sleepwear aids in maintaining a stable core temperature by facilitating the dissipation of excess heat. Example: studies suggest that overheating is a contributing factor in Sudden Infant Death Syndrome (SIDS); breathable sleepwear is considered a preventative measure.
- Comparison to Other Materials
Conventional cotton and synthetic fabrics often exhibit lower breathability compared to bamboo-derived textiles. This difference stems from variations in fiber structure and weaving patterns. Example: tightly woven polyester garments restrict airflow, increasing the risk of heat retention; loosely woven cotton garments offer improved breathability but may lack the moisture-wicking properties of bamboo.
In summary, the breathability inherent in sleepwear made from bamboo-derived material contributes to improved thermal regulation, enhanced moisture management, and a reduced risk of overheating. This characteristic, coupled with other beneficial properties, underscores its relevance in the context of infant well-being and sleep safety. Further investigation into the specific breathability metrics of various textile blends would refine our understanding of optimal material selection.
3. Hypoallergenic
The term “hypoallergenic,” when applied to infant sleepwear, signifies a reduced propensity to cause allergic reactions. Sleepwear crafted from bamboo-derived fabric is frequently marketed as hypoallergenic due to the inherent properties of the fiber and the manufacturing processes employed. The lower likelihood of allergic response is primarily attributed to several factors: the smooth fiber structure, the reduced need for chemical treatments during production, and the natural resistance to dust mites and mold. This attribute is particularly crucial for infants, whose skin is more susceptible to irritation and allergic sensitization. For example, infants with eczema or other skin conditions may experience fewer flare-ups when wearing garments made from this material compared to those made from synthetic fabrics or conventionally processed cotton.
The practical significance of hypoallergenic qualities extends beyond mere comfort. Allergic reactions can disrupt sleep, leading to irritability and impacting overall well-being. Furthermore, chronic exposure to allergens can potentially contribute to the development of more severe allergic conditions later in life. Sleepwear produced with minimal allergenic potential thus serves as a preventative measure, minimizing the risk of adverse reactions. Real-world application can be observed in hospitals and neonatal intensive care units, where sensitive infant skin necessitates the use of materials with documented low allergenicity. Standardized testing procedures exist to assess the hypoallergenic potential of textiles, allowing manufacturers to substantiate their claims and provide consumers with reliable information.
In summary, the connection between hypoallergenic properties and this type of baby sleepwear rests on the fiber’s natural characteristics and production practices. While no material can be guaranteed to be entirely non-allergenic, these garments offer a reduced risk of allergic reactions, making them a suitable choice for infants, especially those with sensitive skin. Continued research into textile allergenicity and improved manufacturing processes will further enhance the safety and comfort of infant apparel.
4. Moisture-wicking
Moisture-wicking, the ability of a fabric to draw moisture away from the skin, is a critical attribute of infant sleepwear. Sleepwear crafted from bamboo-derived material is frequently chosen for its superior moisture-wicking properties, directly influencing the infant’s comfort and reducing the risk of skin irritation and temperature dysregulation. The cause lies in the inherent structure of the fibers, which contain micro-gaps that facilitate the absorption and evaporation of moisture. The importance of this function cannot be overstated: infants are prone to perspiration, and prolonged exposure to dampness can lead to discomfort, skin rashes, and even chilling. Real-life examples include infants who experience night sweats or live in humid climates, where moisture-wicking fabrics can significantly improve sleep quality and prevent skin problems. The practical significance of understanding this lies in the ability to select appropriate sleepwear that promotes a healthier and more comfortable sleep environment for the infant.
Further analysis reveals that the effectiveness of moisture-wicking depends not only on the fiber type but also on the fabric construction. Loosely woven fabrics generally exhibit better moisture-wicking capabilities than tightly woven ones. Moreover, the presence of chemical finishes can either enhance or inhibit moisture-wicking, underscoring the importance of selecting sleepwear certified as free from harmful chemicals. Practical applications include the use of these garments in hospitals, where premature infants require particularly careful management of skin moisture to prevent complications. The selection of appropriate sleepwear, therefore, becomes an integral part of infant care, influencing skin health and overall well-being. Furthermore, this knowledge empowers caregivers to make informed purchasing decisions, prioritizing fabrics with demonstrably superior moisture-wicking properties.
In summary, moisture-wicking is a key determinant of the suitability of this type of infant sleepwear. Its ability to effectively manage moisture contributes to a more comfortable and hygienic sleep environment, reducing the risk of skin irritation and temperature fluctuations. Challenges remain in standardizing the measurement of moisture-wicking and ensuring consistent performance across different brands and blends. Nevertheless, the link between moisture-wicking and the overall well-being of infants highlights the significance of informed fabric selection and proper garment care.
5. Temperature regulation
Temperature regulation is a critical factor in infant well-being, directly influencing sleep quality and overall health. Sleepwear crafted from bamboo-derived fabric is frequently chosen for its perceived ability to aid in temperature regulation, creating a more stable and comfortable sleep environment.
- Fiber Structure and Airflow
The inherent structure of bamboo fibers promotes airflow, facilitating the dissipation of heat. This contrasts with tightly woven synthetic materials that can trap heat, leading to overheating. The increased airflow allows for better ventilation, reducing the likelihood of the infant becoming excessively warm during sleep. For example, in warmer climates, this enhanced breathability can significantly contribute to a more restful sleep.
- Moisture Management and Evaporative Cooling
Bamboo fibers exhibit excellent moisture-wicking properties, drawing perspiration away from the skin. This moisture then evaporates, providing a cooling effect. Effective moisture management is crucial for preventing the infant from becoming chilled due to dampness, particularly in cooler environments. As an example, infants prone to night sweats benefit from this evaporative cooling mechanism.
- Thermal Insulation and Layering
While promoting airflow, bamboo fabric also provides a degree of thermal insulation. This allows for flexible layering, enabling caregivers to adjust the amount of clothing based on ambient temperature. This adaptability is particularly useful in environments with fluctuating temperatures, ensuring the infant remains comfortable throughout the night. A practical example involves adding or removing a lightweight undershirt beneath the sleepwear to accommodate temperature changes.
- Comparison to Alternative Materials
Compared to synthetic fabrics such as polyester, bamboo exhibits superior breathability and moisture-wicking capabilities, leading to enhanced temperature regulation. While cotton offers breathability, it may not possess the same level of moisture-wicking as bamboo. This distinction is significant in maintaining a stable body temperature and preventing discomfort. A clear example would be comparing a bamboo-based sleep sack to one made of fleece, where the bamboo option is more likely to prevent overheating.
The ability of sleepwear made from bamboo-derived fabric to regulate temperature is a key factor in promoting infant comfort and sleep safety. By facilitating airflow, managing moisture, and providing adaptable insulation, these garments contribute to a more stable and comfortable sleep environment. The selection of appropriate sleepwear, therefore, represents a significant aspect of infant care, directly impacting well-being and promoting restful sleep.
6. Durability
Durability, the capacity to withstand wear and tear over an extended period, is a salient characteristic influencing the cost-effectiveness and longevity of infant apparel. Sleepwear crafted from bamboo-derived fabric, while often valued for its softness and breathability, must also exhibit adequate durability to justify its purchase. The connection between this attribute and the material stems from the inherent strength of bamboo fibers and the manufacturing processes employed to create the fabric. Cause-and-effect is evident: stronger fibers and robust construction lead to enhanced durability, translating to a longer lifespan for the garment. The importance of durability is amplified by the frequent washing and usage demands placed on infant clothing. Practical examples include sleepwear retaining its shape and integrity after repeated laundering, resisting pilling, and maintaining seam strength over time. The practical significance of this understanding allows caregivers to make informed purchasing decisions, balancing the benefits of bamboo with the expectation of lasting quality.
Further analysis reveals that durability is not solely determined by the raw material. Weaving patterns, dyeing techniques, and the presence of blended fibers also play crucial roles. Tighter weaves generally enhance durability, while certain dyes and chemical treatments can weaken fibers. Blending bamboo with other materials, such as cotton or spandex, can either increase or decrease durability depending on the properties of the added fiber. Practical applications include the selection of sleepwear with reinforced seams and durable closures, such as snaps or zippers. Real-world examples include observing the performance of different brands of sleepwear after several months of use, noting the extent of fading, shrinkage, and seam integrity. Standardized testing procedures exist to assess fabric durability, providing consumers with objective data to inform their choices. However, anecdotal evidence and long-term user experience remain valuable indicators of overall product lifespan.
In summary, durability is an essential, albeit often overlooked, aspect of infant sleepwear. While the inherent properties of bamboo contribute to a degree of resilience, manufacturing processes and material blends significantly influence the final product’s longevity. Addressing challenges related to standardized durability testing and promoting transparent labeling practices will empower consumers to make more informed decisions. The link between durability and cost-effectiveness underscores the importance of considering this attribute when selecting infant sleepwear, ensuring that garments provide value and utility over an extended period.
7. Sustainability
The connection between sustainability and sleepwear centers on the environmental impact of the materials and production processes involved. The selection of bamboo as the primary fiber is often predicated on its reputation as a sustainable resource, offering potential advantages over conventional cotton and synthetic alternatives. Cause-and-effect is illustrated by the reduced need for pesticides and fertilizers in bamboo cultivation, minimizing environmental contamination. The importance of sustainability stems from the growing awareness of ecological responsibility and the desire to minimize the carbon footprint associated with consumer goods. For example, organic cotton production, while preferable to conventional cotton, still requires significant water resources, whereas bamboo often thrives with minimal irrigation. The practical significance of understanding the eco-friendliness empowers consumers to make environmentally conscious purchasing decisions.
Further analysis reveals that the sustainability of bamboo-derived sleepwear is multifaceted and requires careful scrutiny. The conversion of bamboo into fabric involves chemical processes, and the environmental impact of these processes varies significantly. For instance, the viscose rayon process, commonly used to create bamboo fabric, can release harmful chemicals into the environment if not properly managed. Therefore, certifications such as OEKO-TEX provide assurance that the fabric has been tested for harmful substances and produced in an environmentally responsible manner. Practical applications include seeking sleepwear made from lyocell bamboo, a closed-loop process that minimizes waste and reduces chemical usage. Real-world examples include companies transparently disclosing their manufacturing processes and sourcing practices, allowing consumers to assess the true environmental cost of their purchases. This includes certifications such as the Forest Stewardship Council (FSC) for sustainably sourced bamboo.
In summary, while the use of bamboo in sleepwear offers potential sustainability benefits, a comprehensive assessment of the entire lifecycle, from cultivation to manufacturing and disposal, is essential. Challenges remain in ensuring transparency and accountability throughout the supply chain. However, by prioritizing certified materials, supporting responsible brands, and adopting sustainable laundering practices, consumers can minimize the environmental impact associated with this type of infant apparel. This link between sustainability and infant sleepwear underscores the growing recognition of ecological considerations in consumer choices and promotes responsible consumption patterns.
Frequently Asked Questions
This section addresses common inquiries and clarifies pertinent details regarding sleepwear specifically designed for infants and crafted from bamboo-derived materials.
Question 1: Is bamboo-derived fabric genuinely hypoallergenic?
While frequently marketed as such, “hypoallergenic” lacks a strict regulatory definition. Sleepwear manufactured from this material is often considered less allergenic than synthetic alternatives due to the smooth fiber structure and reduced need for chemical treatments. However, individuals with sensitivities should exercise caution and monitor for reactions.
Question 2: How does the care of this type of sleepwear differ from that of cotton?
Generally, machine washing in cold water and tumble drying on low are recommended. High heat can cause shrinkage and damage the fibers. Specific care instructions may vary by manufacturer; therefore, adherence to the garment label is crucial.
Question 3: Is bamboo fabric truly sustainable?
Sustainability depends on the specific manufacturing processes. Bamboo cultivation itself can be environmentally friendly due to its rapid growth and minimal need for pesticides. However, the conversion of bamboo into fabric, particularly using the viscose process, can involve harsh chemicals. Seeking certifications like OEKO-TEX and lyocell production methods indicates a lower environmental impact.
Question 4: Does this material adequately regulate infant body temperature?
Bamboo-derived fabrics exhibit breathability and moisture-wicking properties, which contribute to temperature regulation. However, appropriate layering remains essential based on ambient temperature. Overheating or chilling can still occur if layering is not carefully considered.
Question 5: What are the potential safety concerns associated with infant sleepwear, regardless of material?
Loose-fitting garments, drawstrings, and decorative embellishments pose potential hazards. Sleepwear should conform to safety standards, including snug-fitting designs or the use of sleep sacks to prevent entanglement and suffocation.
Question 6: How can one verify the authenticity of bamboo-derived fabric?
Labels should clearly state the fiber content. However, misrepresentation can occur. Certifications from reputable organizations, such as those verifying organic or sustainable practices, provide additional assurance of authenticity.
In summary, bamboo-derived infant sleepwear offers several potential benefits, but informed purchasing decisions require a nuanced understanding of the material’s properties and associated considerations.
The subsequent discussion will explore specific product recommendations and highlight reputable brands specializing in this type of infant apparel.
Conclusion
This exploration of bamboo baby sleeper has revealed a confluence of potential benefits and considerations. The inherent softness, breathability, and moisture-wicking properties of bamboo-derived fabrics offer advantages in terms of infant comfort and skin health. Durability and sustainable production practices, while variable, contribute to the overall value proposition. The importance of informed decision-making, considering both the material characteristics and manufacturing processes, is paramount for caregivers.
The future of infant apparel likely involves continued innovation in sustainable materials and manufacturing techniques. As awareness of environmental impact grows, the demand for transparent and ethically produced baby sleepwear is expected to increase. Ongoing research into textile properties and safety standards will further refine the selection process. Prioritizing infant well-being and responsible consumption remains crucial in navigating the complex landscape of baby products.