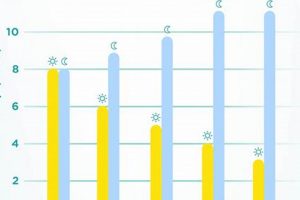
A guide correlating ambient temperature with appropriate clothing and bedding for infants is a resource designed to help caregivers maintain a safe and comfortable sleep environment. For instance, it may suggest a lightweight sleep sack and a room temperature between 68-72 degrees Fahrenheit for optimal infant sleep. This type of visual aid provides guidance on adjusting layers to prevent overheating or chilling.
Maintaining a proper sleep environment contributes significantly to infant well-being by reducing the risk of Sudden Infant Death Syndrome (SIDS), and promoting better sleep quality. Historically, such recommendations were not widely available, potentially increasing the likelihood of unsafe sleep practices. The evolution of these guidelines reflects an increasing understanding of infant thermoregulation and its impact on health outcomes.
Understanding the factors influencing infant sleep safety extends beyond simple temperature readings. Careful consideration of room humidity, the type of bedding materials, and the infant’s individual health conditions are equally important. The following sections will delve into these aspects, providing detailed guidance for caregivers seeking to create an optimal sleep environment.
Optimizing Infant Sleep Environment
Considerations beyond a single temperature reading are crucial when fostering a safe and comfortable sleep environment for infants. The following tips provide actionable guidance:
Tip 1: Monitor Room Temperature. Use a reliable thermometer to accurately assess the ambient temperature in the infant’s sleep area. Aim for a range between 68 and 72 degrees Fahrenheit (20-22 degrees Celsius).
Tip 2: Adjust Clothing Appropriately. Select lightweight, breathable fabrics such as cotton. Avoid overdressing, and consider a single layer more than what an adult would find comfortable in the same environment.
Tip 3: Employ a Wearable Blanket. A properly sized wearable blanket or sleep sack eliminates the need for loose blankets, reducing the risk of suffocation. Ensure the sleep sack is appropriate for the current room temperature.
Tip 4: Avoid Direct Sunlight. Limit direct sunlight exposure in the infant’s sleep area. Excessive solar heat gain can significantly elevate room temperature, even on cooler days.
Tip 5: Consider Room Humidity. Maintain appropriate humidity levels (30-50%) using a humidifier or dehumidifier, as needed. Excessive humidity can exacerbate overheating, while overly dry air can irritate the infant’s airways.
Tip 6: Observe the Infant for Signs of Overheating or Chilling. Look for symptoms such as sweating, rapid breathing, flushed skin (overheating), or shivering, cool extremities, and lethargy (chilling). Adjust clothing and room temperature accordingly.
Tip 7: Ensure Adequate Ventilation. Proper airflow is vital for dissipating heat. Consider using a fan (directed away from the infant) to circulate air, particularly in warmer climates.
Prioritizing environmental factors such as temperature, appropriate clothing, and sufficient ventilation are vital components of safe sleep practices for infants. Consistent application of these guidelines contribute to minimizing risks, particularly those associated with SIDS.
These points serve as a foundation for understanding the significance of controlled environmental conditions during infant sleep. Subsequent sections will elaborate further on specific safety considerations and additional best practices.
1. Optimal room temperature
The concept of “optimal room temperature” is intrinsically linked to the utility of a “baby sleep temperature chart”. These charts provide guidance on how to adjust an infant’s clothing and bedding based on the ambient temperature, with the aim of maintaining thermal comfort and minimizing the risk of overheating or chilling. The suggested “optimal room temperature,” typically between 68-72 degrees Fahrenheit (20-22 degrees Celsius), represents a compromise between preventing hypothermia and avoiding hyperthermia, both of which pose risks to infant health. A higher temperature, for instance, might necessitate fewer layers of clothing, as indicated on the chart, whereas a lower temperature would warrant warmer attire.
The effectiveness of the chart hinges on accurate assessment and maintenance of this temperature. Consider a scenario where a room’s actual temperature deviates significantly from the ideal range due to faulty heating or inadequate ventilation. In such cases, relying solely on the chart without addressing the underlying environmental issue could lead to inappropriate clothing choices, potentially jeopardizing the infant’s thermal regulation. Moreover, variations in individual infants’ physiological responses to temperature necessitate careful observation and adjustments, even within the recommended temperature range.
In summary, while a “baby sleep temperature chart” provides valuable guidelines, its practical application is contingent upon accurately monitoring and regulating the room temperature to fall within the “optimal” range. The chart should be used as a supplementary tool, informed by direct observation of the infant and adjusted based on individual needs. Neglecting the fundamental importance of maintaining the recommended ambient temperature undermines the intended safety benefits of the chart and its associated recommendations.
2. Appropriate clothing layers
The selection of “Appropriate clothing layers” is inextricably linked to the effective use of a “baby sleep temperature chart” in ensuring infant sleep safety. The chart serves as a guide, but the correct application of its recommendations necessitates an understanding of how clothing impacts thermal regulation.
- Fabric Type and Breathability
The material composition of clothing directly influences its breathability and insulation properties. Natural fibers, such as cotton and merino wool, allow for better air circulation compared to synthetic materials like polyester. A “baby sleep temperature chart” might recommend lighter cotton layers in warmer conditions to prevent overheating, while suggesting merino wool in cooler environments to retain warmth. The chart’s efficacy relies on using breathable fabrics to achieve the desired thermal outcome.
- Layering Technique
Layering enables caregivers to adjust insulation based on temperature fluctuations. A “baby sleep temperature chart” may advise multiple thin layers, which can be added or removed, as opposed to a single thick layer. This approach provides greater flexibility in managing the infant’s body temperature. For example, a base layer of a cotton onesie, followed by a lightweight sleep sack, allows for adjustments without fully exposing the infant to colder air.
- Avoiding Overdressing
Overdressing is a significant risk factor for Sudden Infant Death Syndrome (SIDS). A “baby sleep temperature chart” cautions against excessive clothing, emphasizing that infants generally require only one layer more than what an adult would wear comfortably. Overdressing can lead to overheating, characterized by sweating, flushed skin, and rapid breathing. Vigilance and adherence to the chart’s recommendations regarding appropriate layering are crucial in preventing this dangerous scenario.
- Diaper Type Considerations
The type of diaper used can also impact thermal comfort. Cloth diapers, particularly those made from multiple layers of absorbent material, can provide additional insulation around the lower body. This factor should be considered when determining “Appropriate clothing layers” using a “baby sleep temperature chart.” A heavier diaper might warrant reducing the number of clothing layers on the upper body to maintain thermal equilibrium.
In conclusion, the “Appropriate clothing layers” recommendations derived from a “baby sleep temperature chart” necessitate careful consideration of fabric type, layering techniques, the avoidance of overdressing, and even diaper selection. The chart is a tool to inform, but not replace, careful observation and reasoned judgment in ensuring the infant’s thermal comfort and safety.
3. Wearable blanket safety
The implementation of “wearable blanket safety” protocols is inextricably linked to the guidance provided by a “baby sleep temperature chart”. These charts advocate for the use of wearable blankets as a safer alternative to loose bedding, but their efficacy hinges on adhering to strict safety guidelines to mitigate potential risks.
- Proper Sizing and Fit
A properly sized wearable blanket ensures that the infant’s arms and neck are not restricted, preventing potential entanglement or suffocation hazards. A “baby sleep temperature chart” implicitly assumes that the wearable blanket is appropriately sized for the infant’s current weight and length. An ill-fitting garment compromises its safety profile and negates the benefits outlined by the chart.
- Appropriate TOG Rating
The Thermal Overall Grade (TOG) rating of a wearable blanket indicates its insulation level. A “baby sleep temperature chart” often correlates ambient temperature with suggested TOG values for wearable blankets. Using a wearable blanket with an excessively high TOG rating in a warm environment can lead to overheating, contravening the chart’s primary goal of maintaining safe sleep temperatures. Conversely, an inadequate TOG rating in a colder room may result in hypothermia.
- Material Composition and Breathability
The fabric from which a wearable blanket is constructed influences its breathability and moisture-wicking properties. Synthetic materials with poor ventilation can trap heat and moisture, increasing the risk of overheating. “Baby sleep temperature chart” recommendations are predicated on the assumption that the wearable blanket is made from breathable, natural fibers such as cotton or muslin, which facilitate air circulation and reduce the risk of thermal stress.
- Regular Inspection and Maintenance
Wearable blankets should be routinely inspected for signs of wear and tear, such as loose seams, detached fasteners, or compromised fabric integrity. Damaged wearable blankets pose a safety hazard and should be repaired or replaced immediately. A “baby sleep temperature chart” cannot account for the risks associated with damaged or malfunctioning wearable blankets, underscoring the importance of vigilant inspection and maintenance.
The facets of “wearable blanket safety,” encompassing proper sizing, appropriate TOG rating, breathable material composition, and regular inspection, are integral to the successful application of a “baby sleep temperature chart”. Deviation from these safety protocols undermines the intended benefits of the chart and potentially exposes infants to preventable risks. Therefore, adherence to wearable blanket safety guidelines is paramount in ensuring safe and effective utilization of a “baby sleep temperature chart”.
4. Overheating signs
Recognition of “overheating signs” constitutes a critical component of successfully implementing a “baby sleep temperature chart.” The chart provides guidelines for maintaining an appropriate sleep environment; however, its effectiveness depends upon the caregiver’s ability to detect physiological indicators of excessive warmth in the infant. Failure to recognize these signs renders the chart’s recommendations insufficient to ensure safe sleep. For example, if a chart suggests specific clothing layers for a room temperature of 70F, but the infant exhibits sweating and rapid breathing (clear overheating signs), adherence to the chart alone is inadequate. The caregiver must reduce clothing layers regardless of the initial chart recommendation.
The ability to identify “overheating signs” enables proactive intervention to prevent heat stress and reduce the risk of SIDS. Real-life scenarios highlight the practical significance of this understanding. An infant swaddled too tightly or dressed in overly warm clothing in a room with adequate temperature may still overheat due to impaired heat dissipation. Observable signs such as flushed skin, restlessness, and damp hair provide immediate feedback, prompting caregivers to adjust the infant’s attire or environmental conditions. Delayed recognition of these signals can lead to dehydration, lethargy, and potentially, a dangerous elevation of body temperature. The integration of direct observation with the chart’s guidelines is essential for a comprehensive approach to safe infant sleep.
In conclusion, the correlation between “overheating signs” and a “baby sleep temperature chart” underscores the importance of a holistic strategy for maintaining infant thermal safety. While the chart offers a framework for appropriate clothing and room temperature, it is not a substitute for attentive observation of the infant’s physiological state. Challenges arise when caregivers rely solely on the chart without considering individual variations in infant thermoregulation. Therefore, educating caregivers about “overheating signs” and emphasizing their role in conjunction with chart recommendations is crucial for promoting safe infant sleep practices and minimizing the risk of adverse outcomes.
5. Chilling indicators
The correlation between observable “chilling indicators” and a “baby sleep temperature chart” is crucial for maintaining a safe and comfortable sleep environment for infants. While the chart provides guidelines for appropriate clothing and room temperature, it is imperative to recognize physiological signs indicating that an infant is too cold, irrespective of adherence to the chart’s recommendations. Overreliance on the chart without acknowledging “chilling indicators” can lead to hypothermia and other adverse outcomes.
- Cool Extremities and Body Core
Tactile assessment of the infant’s extremities (hands and feet) and body core is essential. Coolness to the touch, especially when accompanied by pallor or mottling of the skin, suggests inadequate warmth. A “baby sleep temperature chart” may suggest a specific layering strategy, but if the infant’s extremities remain cool, additional layers or a higher TOG-rated wearable blanket may be necessary to restore thermal balance. This assessment overrides the chart’s recommendation, placing precedence on the infant’s physiological state.
- Shivering or Tremors
Shivering is an involuntary muscular contraction intended to generate heat. While shivering is less common in infants compared to adults, subtle tremors or jerky movements can indicate an attempt to increase body temperature. If these “chilling indicators” are observed, immediate action is required, even if the “baby sleep temperature chart” suggests the current clothing is appropriate. The observation of shivering demonstrates a clear need for increased insulation.
- Lethargy and Decreased Activity
Hypothermia can lead to decreased activity and lethargy in infants. A normally active infant who becomes unusually quiet or unresponsive may be experiencing a drop in body temperature. Caregivers should assess other “chilling indicators” concurrently and promptly increase the infant’s warmth, even if the room temperature aligns with the “baby sleep temperature chart’s” recommended range. Reduced activity level may signify a critical need for intervention.
- Changes in Breathing Pattern
In severe cases of hypothermia, infants may exhibit changes in their breathing pattern, such as slow or shallow respirations. This is a late-stage indicator requiring immediate medical attention. While a “baby sleep temperature chart” aims to prevent such occurrences, caregivers must be vigilant for any respiratory changes, as they signal a serious compromise to the infant’s physiological stability, necessitating immediate action beyond simply adjusting the sleep environment according to the chart.
In summary, while “baby sleep temperature charts” offer helpful guidance for maintaining an appropriate sleep environment, recognition of “chilling indicators” is paramount. Caregivers must prioritize direct observation of the infant’s physiological state and be prepared to deviate from the chart’s recommendations to address individual needs. The chart serves as a tool, but direct assessment and responsiveness to “chilling indicators” are essential for ensuring infant safety and well-being.
6. Humidity considerations
Environmental humidity plays a significant role in infant thermal regulation and, consequently, influences the effective application of a “baby sleep temperature chart.” While the chart provides guidelines for temperature and clothing, humidity levels can significantly alter how an infant perceives and responds to a given temperature, impacting safety and comfort.
- Impact on Evaporative Cooling
Evaporation of sweat is a primary mechanism for cooling the body. High humidity inhibits evaporation, reducing the body’s ability to dissipate heat. A “baby sleep temperature chart” may recommend specific clothing for a given temperature, but in high humidity, this recommendation may lead to overheating, as the infant’s natural cooling mechanisms are compromised. For instance, a room temperature of 72F with 80% humidity can feel significantly warmer and more oppressive than the same temperature with 40% humidity, necessitating lighter clothing than suggested solely by temperature readings.
- Respiratory Health Implications
Both excessively high and low humidity levels can negatively affect infant respiratory health. High humidity promotes the growth of mold and dust mites, potentially exacerbating allergies and asthma. Conversely, low humidity can dry out nasal passages and mucous membranes, increasing susceptibility to respiratory infections. These health considerations interact with the use of a “baby sleep temperature chart” because respiratory distress can alter an infant’s thermal comfort and regulation, requiring adjustments to clothing and bedding regardless of the temperature guidelines.
- Influence on Perceived Comfort
Infant comfort is not solely determined by temperature; humidity also plays a critical role. An environment within the temperature range recommended by a “baby sleep temperature chart” may still be uncomfortable if the humidity is excessively high or low. For example, a dry room might cause skin irritation and discomfort, even if the temperature is optimal. This discomfort can disrupt sleep patterns and impact overall well-being, highlighting the need to consider humidity as an independent factor when assessing the sleep environment.
- Measurement and Adjustment Strategies
Accurate monitoring of humidity levels is essential for informed decision-making regarding infant sleepwear and bedding. Hygrometers provide a means of measuring ambient humidity. If humidity levels deviate significantly from the recommended range (30-50%), adjustments should be made using humidifiers or dehumidifiers. Integrating humidity measurements into the decision-making process alongside the “baby sleep temperature chart” ensures a more comprehensive approach to creating a safe and comfortable sleep environment.
These considerations underscore that the effective implementation of a “baby sleep temperature chart” requires a holistic approach. Focusing solely on temperature without accounting for humidity can lead to inaccurate assessments of infant thermal comfort and compromise sleep safety. Addressing both temperature and humidity optimizes the sleep environment, promoting infant well-being and minimizing potential health risks.
7. Consistent monitoring
The effective utilization of a “baby sleep temperature chart” necessitates “consistent monitoring” of both the ambient environment and the infant’s physiological state. These charts offer generalized guidelines regarding appropriate clothing and bedding; however, the dynamic interplay between external temperature, humidity, and individual infant characteristics demands continuous assessment. Without vigilant observation, adherence to a static chart can be misleading, potentially leading to either overheating or chilling, despite seemingly following recommended practices. For instance, a chart may suggest a specific layering configuration for a 70F room, but if unmonitored, a sudden increase in room temperature due to sunlight exposure could render that configuration dangerous. “Consistent monitoring” acts as a critical feedback loop, allowing caregivers to proactively adjust the sleep environment and attire in response to real-time conditions.
The practical significance of “consistent monitoring” extends beyond merely checking a thermometer. It involves actively observing the infant for signs of thermal distress. These signs can include sweating, flushed skin, rapid breathing, or restlessness (indicating overheating), as well as cool extremities, shivering, or lethargy (suggesting chilling). “Consistent monitoring” further entails periodically reassessing room temperature and humidity levels, accounting for fluctuations throughout the day and night. A reliance solely on a pre-determined chart without considering these dynamic factors undermines its intended safety benefits. Consider a scenario where a caregiver adheres to the chart’s recommendations but fails to notice that the infant’s hands and feet are consistently cool. In this case, “consistent monitoring” would prompt the addition of extra socks or a warmer sleep sack, even if the overall room temperature aligns with the chart’s guidelines.
In conclusion, “consistent monitoring” is not merely an adjunct to using a “baby sleep temperature chart” but an indispensable component of a comprehensive safe sleep strategy. Challenges arise when caregivers view the chart as a fixed prescription rather than a dynamic guideline. Successful implementation requires integrating the chart’s recommendations with ongoing assessment of both the sleep environment and the infant’s physiological response. By prioritizing “consistent monitoring,” caregivers can proactively mitigate risks associated with thermal imbalance and ensure a safer and more comfortable sleep experience for infants. The ultimate goal remains adapting the sleep environment to meet the individual needs of the infant, with the chart serving as a valuable but not absolute reference point.
Frequently Asked Questions
The following questions address common concerns and misconceptions regarding infant sleep temperature management and the appropriate use of resources intended to provide guidance in this area.
Question 1: How accurate are general recommendations provided in a “baby sleep temperature chart” given individual differences in infant thermoregulation?
A “baby sleep temperature chart” offers general guidelines. Individual variations in metabolism, activity level, and body composition influence an infant’s thermoregulatory capacity. Direct observation of the infant for signs of overheating or chilling is essential, overriding chart recommendations if necessary.
Question 2: Is it possible to solely rely on a “baby sleep temperature chart” to ensure safe sleep practices, or are there other risk factors to consider?
Reliance on a “baby sleep temperature chart” alone is insufficient for ensuring safe sleep. Other factors, including sleeping position (back is safest), firm sleep surface, avoidance of soft bedding, and a smoke-free environment, must also be considered. The chart addresses one element of a comprehensive safe sleep strategy.
Question 3: What is the appropriate course of action if an infant consistently exhibits signs of overheating or chilling, despite adhering to the guidelines in a “baby sleep temperature chart”?
Consistent signs of thermal distress, despite following a “baby sleep temperature chart,” warrant consultation with a pediatrician. Underlying medical conditions may affect an infant’s thermoregulation. Further medical evaluation may be required.
Question 4: Can the “baby sleep temperature chart” be used as a reference for infants with specific health conditions, such as prematurity or respiratory issues?
Infants with prematurity or respiratory issues may have compromised thermoregulation. While a “baby sleep temperature chart” provides a general framework, individualized recommendations from a healthcare professional are necessary to account for their specific needs.
Question 5: How frequently should temperature and humidity levels be checked in the infant’s sleep environment when using a “baby sleep temperature chart”?
Regular monitoring is necessary due to fluctuations in ambient conditions. Checking temperature and humidity levels at least twice daily, and more frequently during periods of significant weather changes, is advisable to ensure the infant’s comfort and safety.
Question 6: Are there any potential limitations or drawbacks to using a “baby sleep temperature chart” that caregivers should be aware of?
A potential drawback is over-reliance on the chart without individual assessment. The chart is a tool, not a substitute for parental observation and judgment. Misinterpretation of chart recommendations or failure to account for individual variations can compromise infant safety.
The information provided serves as a general guide and should not replace professional medical advice. Consult with a qualified healthcare provider for personalized recommendations regarding infant sleep practices.
The subsequent sections will expand on these points, offering practical tips for creating a safer and more comfortable sleep environment for infants.
Conclusion
The preceding discussion clarifies the role of a “baby sleep temperature chart” as a supportive, but not definitive, tool for promoting infant sleep safety. It emphasizes the critical interplay between environmental monitoring, physiological observation, and informed judgment. Over-reliance on prescriptive guidelines without considering individual infant needs or dynamic environmental conditions can undermine the intended safety benefits. Recognition of overheating and chilling indicators, coupled with adjustments based on real-time assessments, constitutes a more comprehensive approach.
Ultimately, responsible utilization of a “baby sleep temperature chart” hinges on a commitment to proactive and informed caregiving. Continued research and dissemination of evidence-based practices remain vital for advancing infant sleep safety. Vigilance, education, and responsiveness are paramount in creating an environment conducive to both infant well-being and parental peace of mind. This necessitates moving beyond a passive adherence to external directives toward an active engagement in understanding and responding to the unique needs of each infant.