A delayed sleep onset, specifically when an infant consistently resists falling asleep until late in the evening, such as 11 PM, represents a common challenge for many parents. This situation often involves prolonged periods of crying, fussing, or wakefulness in the crib, despite attempts to establish a regular bedtime routine. For example, a caregiver might consistently put the child to bed around 8 PM, only to have the infant remain awake and restless for several hours before finally falling asleep.
Addressing a child’s late sleep time offers significant benefits for both the infant and the family. Early and consistent sleep schedules are crucial for optimal cognitive and physical development in infants. Furthermore, establishing a more reasonable bedtime allows parents to regain valuable evening hours, reducing stress and improving overall family well-being. Historically, cultures have employed various techniques, from swaddling to lullabies, to promote infant sleep, reflecting the long-standing recognition of the importance of regular sleep patterns.
Consequently, this discussion will focus on identifying the underlying causes contributing to this late sleep onset, evaluating effective strategies for adjusting an infant’s sleep schedule, and exploring methods for creating a sleep-conducive environment. This approach aims to provide practical guidance for parents navigating this frequently encountered phase of infant development.
Strategies for Addressing a Late Infant Bedtime
Establishing a more appropriate sleep schedule for an infant who consistently delays sleep until late in the evening requires a multifaceted approach that addresses both behavioral and environmental factors.
Tip 1: Evaluate the Daytime Napping Schedule: Excessive or poorly timed daytime naps can interfere with nighttime sleep. Analyze the duration and timing of naps to ensure they do not extend too close to bedtime. For example, limiting a late afternoon nap or shortening its duration may improve the likelihood of earlier sleep onset.
Tip 2: Implement a Consistent Bedtime Routine: A predictable sequence of calming activities prior to bedtime signals to the infant that it is time to sleep. This routine could include a bath, gentle massage, reading a story, and quiet singing. Consistency in the order and timing of these activities is essential for establishing a sleep association.
Tip 3: Optimize the Sleep Environment: The infant’s sleep environment should be conducive to sleep. This includes ensuring a dark, quiet, and cool room. Consider using blackout curtains, a white noise machine, or a fan to minimize distractions and create a calming atmosphere.
Tip 4: Gradual Bedtime Adjustment: Abrupt changes to bedtime can be disruptive. Instead, gradually shift bedtime earlier by 15-30 minutes each night until the desired bedtime is reached. This gradual adjustment allows the infant to adapt more easily to the new schedule.
Tip 5: Monitor Feeding Patterns: Ensure the infant is adequately fed during the day to minimize nighttime hunger. However, avoid feeding the infant immediately before bedtime, as this can create a sleep association that requires feeding to fall asleep. Consider offering a final feeding at least 30 minutes before the start of the bedtime routine.
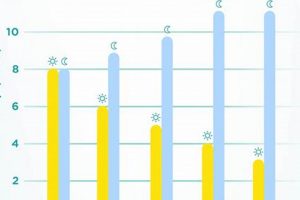
Tip 6: Consistent Wake-Up Time: Maintaining a consistent wake-up time, even on weekends, helps regulate the infant’s circadian rhythm and promotes more predictable sleep patterns. Exposing the infant to natural light shortly after waking can further reinforce the sleep-wake cycle.
Implementing these strategies consistently can promote a more desirable infant sleep schedule, leading to improved sleep for both the infant and the caregivers. This proactive approach contributes to enhanced well-being and developmental progress.
These guidelines provide a foundation for addressing delayed infant sleep onset. Further discussion will address potential medical factors and when professional consultation may be necessary.
1. Circadian Rhythm
The circadian rhythm, an internal biological clock regulating the sleep-wake cycle, plays a fundamental role in determining an infant’s sleep patterns. When an infant habitually resists falling asleep until late, such as 11 PM, it frequently indicates a misalignment or disruption of this inherent timing system. This misalignment can manifest as a delayed phase in the circadian rhythm, causing the infant’s body to naturally feel alert and awake during the hours when sleep is desired. For example, consistent exposure to bright lights or stimulating activities in the evening can suppress melatonin production, a hormone crucial for inducing sleepiness, thereby perpetuating a later sleep onset.
The importance of the circadian rhythm as a key component in addressing delayed sleep onset lies in its ability to influence the timing of sleep-related hormones and physiological processes. When an infant’s internal clock is synchronized with the external environment, they typically experience a natural increase in sleepiness during the evening hours. Conversely, disruption of this synchrony can lead to difficulties falling asleep and maintaining sleep throughout the night. Consider a situation where an infant is consistently exposed to screen time before bed; the blue light emitted from electronic devices can suppress melatonin secretion, effectively shifting the circadian rhythm later and making it challenging for the infant to fall asleep at an earlier hour. Understanding the circadian rhythm allows caregivers to implement strategies aimed at realigning the infant’s internal clock with the desired sleep schedule.
In conclusion, the link between the circadian rhythm and a late bedtime is undeniable. By understanding and addressing disruptions to the circadian rhythm, caregivers can begin to improve infant sleep patterns. Re-establishing circadian rhythm entrainment may require carefully planned light exposure, consistent wake and sleep times, and strategic timing of activities. The challenges involve the dedication and effort required to implement these changes consistently and patiently over time. Restoring a healthy circadian rhythm ultimately contributes to improved sleep quality and overall health outcomes for the infant.
2. Sleep Environment
The sleep environment exerts a profound influence on an infant’s ability to fall asleep and maintain sleep throughout the night. In cases where an infant consistently resists sleep until late in the evening, such as 11 PM, a critical assessment of the sleep environment is warranted to identify and address potential impediments to sleep onset.
- Light Exposure
Excessive light exposure, particularly in the evening hours, can suppress melatonin production and disrupt the circadian rhythm, delaying sleep onset. Bright lights from electronic devices, overhead lighting, or even streetlights entering the room can interfere with the body’s natural sleep signals. For example, an infant exposed to a brightly lit room before bed may experience difficulty falling asleep and may remain awake and restless until significantly later in the evening. Minimizing light exposure in the hours leading up to bedtime and ensuring a dark sleep environment are essential for promoting sleep.
- Noise Levels
Excessive noise can be a significant barrier to infant sleep. Loud noises, such as television sounds, conversations, or traffic noise, can disrupt sleep onset and awaken the infant during the night. For instance, an infant living in a noisy urban environment may struggle to fall asleep early and may experience frequent awakenings due to external disturbances. Creating a quiet sleep environment through the use of white noise machines or soundproofing measures can help mask distracting noises and promote more restful sleep.
- Temperature and Ventilation
An uncomfortable room temperature can negatively impact an infant’s ability to fall asleep. Both excessive warmth and excessive cold can disrupt sleep and lead to restlessness. For example, an infant in an overheated room may become uncomfortable and struggle to fall asleep, while an infant in a cold room may wake up frequently due to feeling chilled. Maintaining a comfortable and consistent room temperature, typically between 68-72 degrees Fahrenheit, is crucial for promoting optimal sleep. Adequate ventilation is also important to prevent the room from becoming stuffy or stale.
- Comfort and Safety
A safe and comfortable sleep environment is essential for infant sleep. This includes ensuring the crib or bassinet meets safety standards, using a firm mattress, and avoiding loose bedding, pillows, and soft toys that pose a suffocation risk. For example, an infant placed to sleep on a soft mattress with loose blankets may be at increased risk of sudden infant death syndrome (SIDS) and may also experience discomfort that disrupts sleep. Prioritizing safety and comfort in the sleep environment is paramount for promoting restful sleep and minimizing risk.
These elements of the sleep environment are interwoven and contribute to an infant’s ability to fall asleep at an appropriate time. By carefully assessing and optimizing the sleep environment, caregivers can improve the likelihood of earlier sleep onset and promote healthier sleep habits. Addressing these environmental factors can often be an essential step in resolving the issue of an infant resisting sleep until late in the evening.
3. Daytime Naps
Daytime naps significantly influence an infant’s nighttime sleep patterns. The duration, timing, and frequency of these naps directly impact the ease with which an infant transitions to sleep in the evening. In cases where infants consistently resist falling asleep until late, such as 11 PM, a thorough evaluation of daytime napping habits becomes essential.
- Nap Duration
Excessively long daytime naps can diminish the infant’s drive to sleep at night. The cumulative effect of prolonged daytime sleep reduces the build-up of sleep pressure, a physiological process that promotes sleepiness. For example, if an infant sleeps for several hours during the day, they may not feel sufficiently tired by a typical bedtime, contributing to resistance and delayed sleep onset. Monitoring the total amount of daytime sleep is crucial for regulating nighttime sleep.
- Nap Timing
The timing of daytime naps relative to bedtime is equally important. Late afternoon or evening naps can significantly interfere with nighttime sleep. A nap that concludes too close to bedtime may prevent the infant from developing sufficient sleep pressure before the evening, resulting in difficulty falling asleep at a desired time. For instance, an infant who naps until 6 PM will likely not be ready for sleep by 8 PM or 9 PM, leading to a prolonged period of wakefulness and resistance to bedtime. Adjusting nap schedules to conclude earlier in the afternoon can promote earlier sleep onset at night.
- Nap Frequency
The number of naps an infant takes during the day also affects nighttime sleep. While infants require daytime sleep, too many naps can disrupt the consolidation of sleep patterns. Fragmented sleep schedules with frequent short naps may prevent the infant from developing a consistent sleep-wake cycle. Infants who take several short naps throughout the day might not experience the same level of sleepiness at bedtime as those on a more consolidated nap schedule. Regulating the number of naps to promote longer periods of wakefulness during the day can enhance the drive to sleep at night.
- Consistency of Nap Schedule
Inconsistency in the nap schedule can lead to unpredictable sleep patterns. A variable nap schedule, where the timing and duration of naps fluctuate daily, can disrupt the infant’s circadian rhythm and make it difficult to establish a consistent bedtime. For example, if an infant’s nap times vary significantly from day to day, they may not develop a predictable sense of when sleep is expected, contributing to bedtime resistance and delayed sleep onset. Establishing a more consistent nap schedule, even within a range of acceptable times, can help regulate the infant’s internal clock and promote more predictable sleep patterns.
The connection between daytime naps and a late bedtime is complex and multifaceted. By carefully considering the duration, timing, frequency, and consistency of daytime naps, caregivers can better understand and address the underlying causes of delayed sleep onset. Modifying these aspects of the nap schedule can promote a more favorable sleep-wake cycle and contribute to improved nighttime sleep for the infant.
4. Bedtime Routine
A consistent and carefully designed bedtime routine plays a critical role in establishing healthy sleep patterns for infants. The absence or inadequacy of such a routine is frequently implicated when an infant consistently resists sleep until late in the evening, such as 11 PM. A predictable sequence of events preceding bedtime serves as a signal, preparing the infant both physically and psychologically for sleep.
- Predictability and Sleep Associations
A structured bedtime routine allows the infant to form strong associations between specific activities and the impending sleep. This predictability reduces anxiety and resistance, as the infant anticipates the transition to sleep. For example, if the routine consistently includes a warm bath, a story, and quiet singing, the infant learns to associate these activities with the expectation of sleep. The lack of such a routine can lead to confusion and uncertainty, making it difficult for the infant to settle down.
- Calming Activities and Physiological Relaxation
Effective bedtime routines prioritize calming activities that promote physiological relaxation. These activities help to reduce stimulation and prepare the infant’s body for sleep. Examples include gentle massage, quiet reading, and soft music. Conversely, activities that are overly stimulating, such as active play or screen time, should be avoided, as they can increase alertness and delay sleep onset. A routine focused on relaxation facilitates the transition to sleep.
- Timing and Consistency
The timing and consistency of the bedtime routine are crucial. The routine should occur at the same time each evening, creating a predictable rhythm that reinforces the infant’s circadian rhythm. Furthermore, the sequence of activities should remain consistent to strengthen the sleep associations. For instance, a routine that begins with a bath at 7:30 PM and concludes with bedtime at 8:00 PM should be maintained consistently. Variations in timing or activities can disrupt the infant’s expectations and lead to resistance.
- Individualization and Adaptation
While a consistent structure is essential, the specific activities included in the bedtime routine should be tailored to the individual infant’s needs and preferences. What works for one infant may not work for another. Caregivers must observe the infant’s cues and adapt the routine accordingly. For example, some infants may find a specific type of music soothing, while others may prefer a quiet environment. A routine that is tailored to the infant’s individual needs is more likely to be effective in promoting sleep.
The effectiveness of a bedtime routine in addressing a late bedtime hinges on its predictability, calming nature, consistent timing, and individualization. When implemented thoughtfully and consistently, a well-designed bedtime routine can significantly improve an infant’s ability to fall asleep at an appropriate time. Conversely, the absence or inconsistent application of such a routine frequently contributes to the problem of an infant resisting sleep until late in the evening. Creating and adhering to a solid bedtime routine may be required in order to address a late infant bedtime.
5. Feeding Schedule
The infant feeding schedule is intricately connected to sleep patterns and can significantly contribute to a delayed bedtime, such as consistently resisting sleep until 11 PM. An infant’s nutritional intake and the timing of feeds influence sleep onset and maintenance. Understanding this relationship is crucial for addressing sleep disturbances.
- Nutritional Adequacy and Satiety
Inadequate caloric intake during the day can lead to nighttime hunger, causing the infant to awaken or resist falling asleep until fed. Insufficient daytime feeding necessitates nighttime feeds, potentially delaying sleep onset. For example, an infant who does not receive sufficient breast milk or formula during the day may experience hunger pangs in the evening, resulting in fussiness and difficulty settling down for sleep. Ensuring the infant receives appropriate nutrition throughout the day can reduce nighttime hunger and promote earlier sleep.
- Timing of the Last Feeding
The timing of the final feeding relative to bedtime impacts sleep onset. Feeding immediately before bedtime can create a dependency, where the infant associates feeding with falling asleep. This association may lead to the infant resisting sleep if not fed, even if not truly hungry. Furthermore, lying down immediately after feeding can cause discomfort due to reflux, further disrupting sleep. For instance, an infant who is consistently fed right before being placed in the crib may become accustomed to this practice and resist sleep without it. Separating the last feeding from bedtime by at least 30 minutes can mitigate these issues.
- Type of Feeding (Breast Milk vs. Formula)
While both breast milk and formula provide essential nutrition, they are digested at different rates. Breast milk is generally digested more quickly than formula, potentially leading to earlier hunger cues. This difference can affect the frequency of nighttime feedings and subsequently influence sleep patterns. For example, a breastfed infant may require more frequent feedings than a formula-fed infant, especially during growth spurts. Understanding the digestion characteristics of the chosen feeding method can help anticipate and manage nighttime feeding needs.
- Feeding Schedules and Circadian Rhythm
Consistent feeding schedules can help regulate an infant’s circadian rhythm and promote more predictable sleep patterns. Irregular feeding times can disrupt the internal clock, making it difficult for the infant to establish a consistent sleep-wake cycle. For instance, an infant fed at varying times each day may experience inconsistent sleep patterns, contributing to delayed sleep onset. Establishing a predictable feeding schedule, aligned with natural hunger cues, can help synchronize the circadian rhythm and improve sleep patterns.
The interplay between feeding schedule and infant sleep is undeniable. By addressing nutritional adequacy, timing the last feeding appropriately, understanding the characteristics of the feeding method, and establishing a consistent schedule, caregivers can significantly influence sleep patterns and potentially resolve the issue of an infant resisting sleep until late in the evening. These feeding strategies work in concert with other sleep hygiene practices to establish a healthy sleep-wake cycle.
6. Underlying Conditions
Certain medical or developmental conditions can manifest as sleep disturbances, contributing to an infants resistance to sleep until late in the evening. These underlying conditions directly affect the infant’s physiological state, neurological function, or level of comfort, thereby impacting sleep onset and maintenance. For example, an undiagnosed food allergy or intolerance can cause gastrointestinal discomfort, leading to fussiness and difficulty settling down for sleep. Similarly, conditions like eczema, characterized by itchy skin, can disrupt sleep due to discomfort and the urge to scratch. The existence of such underlying issues underscores the importance of medical evaluation when behavioral interventions alone are insufficient.
Consider the case of an infant experiencing undiagnosed reflux. The discomfort caused by stomach acid backing up into the esophagus can lead to frequent awakenings and resistance to lying down for sleep. Infants with developmental delays, such as sensory processing issues, may also exhibit atypical sleep patterns, including resistance to sleep and prolonged periods of wakefulness. In these instances, addressing the underlying medical or developmental condition is paramount. Medical interventions, such as dietary changes for food allergies or medication for reflux, may be necessary to alleviate symptoms and promote healthier sleep patterns. Similarly, therapeutic interventions, such as occupational therapy for sensory processing issues, can help improve an infant’s ability to regulate their arousal levels and transition to sleep.
In summary, underlying medical and developmental conditions should be considered when an infant consistently resists sleep until late in the evening. Ignoring these potential factors can lead to ineffective interventions and prolonged sleep disturbances. A thorough medical evaluation, coupled with appropriate medical or therapeutic interventions, is often necessary to address the root cause of the sleep problem and improve infant sleep patterns. Early identification and management of these underlying conditions can significantly contribute to the infant’s overall well-being and family quality of life.
Frequently Asked Questions
The following questions address common concerns regarding infants who consistently resist falling asleep until late in the evening.
Question 1: At what age is an 11 PM bedtime considered a problem for an infant?
While individual sleep needs vary, a consistent 11 PM bedtime is generally considered problematic for infants of most ages. Infants require significantly more sleep than adults, and a late bedtime can interfere with their developmental needs, regardless of age. A more age-appropriate bedtime, typically between 7 PM and 9 PM, is generally recommended to ensure adequate sleep duration and consolidation.
Question 2: What are the potential long-term consequences of a consistently late bedtime for an infant?
Chronic sleep deprivation due to a consistently late bedtime can have several long-term consequences for infants. These may include impaired cognitive development, behavioral problems, weakened immune function, and an increased risk of obesity. Adequate sleep is crucial for brain development and overall well-being, making it essential to address and correct persistent sleep disturbances.
Question 3: Can teething contribute to an infant’s resistance to falling asleep until late?
Teething can indeed contribute to sleep disturbances in infants, including resistance to falling asleep. The discomfort associated with teething, such as gum inflammation and pain, can make it difficult for the infant to settle down and sleep soundly. However, teething is often a temporary issue, and other factors contributing to late sleep onset should also be considered.
Question 4: Are there any medical conditions that commonly lead to infants resisting sleep until late?
Several medical conditions can disrupt infant sleep patterns and contribute to late sleep onset. These include gastroesophageal reflux disease (GERD), food allergies or intolerances, eczema, and sleep apnea. These conditions can cause discomfort or breathing difficulties that interfere with sleep. A medical evaluation is warranted if underlying medical issues are suspected.
Question 5: How can a parent distinguish between normal infant fussiness and a more serious sleep problem?
Normal infant fussiness typically occurs in brief episodes and is often related to hunger, diaper changes, or social interaction. A more serious sleep problem is characterized by persistent resistance to sleep, frequent nighttime awakenings, and daytime irritability or fatigue. If an infant consistently struggles to fall asleep or stay asleep, it is essential to seek professional guidance.
Question 6: What professional help is available for parents struggling with an infant who resists sleep until late?
Several professionals can provide support and guidance for parents struggling with infant sleep problems. These include pediatricians, sleep specialists, and certified sleep consultants. These professionals can assess the infant’s sleep patterns, identify underlying causes, and recommend appropriate interventions, such as behavioral strategies or medical treatments.
The answers to these frequently asked questions highlight the complexities of infant sleep and underscore the importance of addressing sleep disturbances proactively.
The next section will provide a recap of the key information covered in this article.
“Baby Won’t Go To Sleep Until 11pm”
The persistent challenge of an infant consistently refusing sleep until late in the evening demands a comprehensive understanding of multifaceted contributing factors. These encompass circadian rhythm disruption, suboptimal sleep environment, inadequate management of daytime naps, inconsistent bedtime routines, and inappropriate feeding schedules. Furthermore, the possibility of underlying medical or developmental conditions exacerbating sleep disturbances necessitates careful consideration. Effective intervention requires a holistic approach addressing these elements in tandem, rather than in isolation.
Addressing the issue of “baby won’t go to sleep until 11pm” is not merely a matter of parental convenience; it directly impacts the infant’s neurological development, physiological well-being, and overall quality of life. Sustained efforts to establish age-appropriate sleep patterns are paramount. Persistent sleep disturbances warrant professional consultation to rule out underlying conditions and formulate targeted intervention strategies. The implications of inaction extend beyond immediate fatigue, potentially shaping the infant’s long-term health trajectory. Prioritizing infant sleep is an investment in their future well-being and a responsibility demanding diligence and informed action.