Infant nutrition products formulated without lactose are designed for babies who experience difficulty digesting this naturally occurring sugar found in milk. These specialized formulas replace lactose with alternative carbohydrates, such as corn syrup solids or sucrose, ensuring provision of essential nutrients necessary for growth and development. These formulas are typically recommended by pediatricians or healthcare professionals for infants exhibiting symptoms like gas, bloating, diarrhea, or fussiness potentially linked to lactose intolerance or sensitivity.
The availability of these modified products plays a critical role in supporting the healthy development of infants who cannot comfortably digest standard milk-based formulas. The absence of lactose allows for improved digestion and nutrient absorption, alleviating discomfort and promoting overall well-being. Historically, the development of these formulations addressed a significant gap in infant nutrition, providing a viable alternative for families seeking relief from lactose-related digestive issues in their babies. This innovation has significantly improved the quality of life for many infants and their caregivers.
The subsequent sections will delve into the specific ingredients commonly found in these specialized formulas, explore the differences between various brands and product types, and outline the steps parents and caregivers should take when considering a switch to this type of feeding option. Additionally, this article will examine the potential long-term implications of using such a formula and offer guidance on addressing any related health concerns.
Guidance on the Use of Lactose-Free Infant Formula
The following guidelines provide information for parents and caregivers considering or currently using infant formulas designed without lactose.
Tip 1: Consult a Healthcare Professional: Prior to initiating the use of this type of formula, a consultation with a pediatrician or registered dietitian is essential. A healthcare professional can accurately assess the infant’s symptoms, diagnose potential lactose intolerance or sensitivity, and determine if a lactose-free formula is the appropriate course of action.
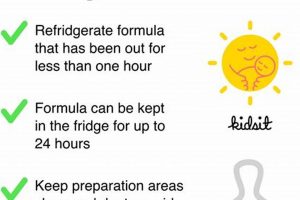
Tip 2: Introduce Gradually: When transitioning to a lactose-free formula, introduce it gradually. Mixing increasing amounts of the new formula with the existing formula over several days can help minimize digestive upset during the adaptation period.
Tip 3: Observe for Changes: Closely monitor the infant for any changes in stool consistency, frequency, or behavior. While the goal is improvement, noting any adverse reactions and communicating them to the healthcare provider is important.
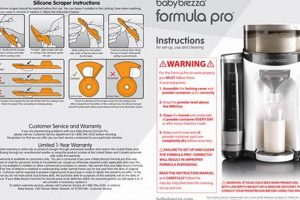
Tip 4: Follow Preparation Instructions: Adhere strictly to the preparation instructions provided on the formula packaging. Improper mixing or dilution can affect the nutritional content and potentially cause digestive issues.
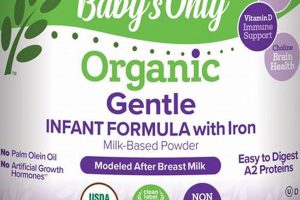
Tip 5: Be Mindful of Ingredients: Scrutinize the ingredient list. While labeled as lacking lactose, formulas may contain other potential allergens or ingredients that do not agree with the infant’s digestive system. Discuss any concerns with the pediatrician.
Tip 6: Ensure Adequate Nutrition: Verify that the chosen formula provides complete and balanced nutrition, meeting the infant’s needs for growth and development. Compare nutritional information with that of standard infant formulas and discuss any concerns with a healthcare professional.
Tip 7: Consider Hydrolyzed Formulas: In some instances, even formulas without lactose may not fully alleviate symptoms. Consider exploring extensively hydrolyzed formulas, where proteins are broken down into smaller, more easily digestible components. Consultation with a pediatrician is vital before making this change.
Consistent implementation of these guidelines promotes optimal infant health and well-being during the use of these specialized formulas.
The following section will explore frequently asked questions related to these formulas, providing further clarity and addressing common concerns.
1. Digestive Symptom Relief
Digestive symptom relief is a primary objective in utilizing infant formulas designed without lactose. Lactose intolerance or sensitivity can manifest in infants as a range of digestive discomforts. Specialized formulas aim to alleviate these symptoms, thereby promoting improved infant well-being.
- Reduction of Gas and Bloating
Infants with lactose intolerance often experience excessive gas production and abdominal bloating due to the undigested lactose fermenting in the gut. Replacing lactose with alternative carbohydrates reduces the substrate for fermentation, thus lessening gas production and bloating. This contributes to a calmer and more comfortable infant.
- Alleviation of Diarrhea
Lactose malabsorption can lead to osmotic diarrhea, where undigested lactose draws water into the intestines. The exclusion of lactose in these formulas helps to normalize bowel movements and reduce the frequency and liquidity of stools. This is particularly important in preventing dehydration and maintaining proper electrolyte balance.
- Mitigation of Fussiness and Irritability
Digestive discomfort from gas, bloating, and diarrhea can contribute to increased fussiness and irritability in infants. By addressing the underlying digestive issues, these formulas can lead to a reduction in crying and an improvement in the infant’s overall mood and demeanor. This benefit is particularly valuable for both the infant and the caregivers.
- Improvement in Nutrient Absorption
When lactose is not properly digested, it can interfere with the absorption of other essential nutrients. Utilizing a formula without lactose allows for better digestion and absorption of fats, proteins, and other micronutrients, ensuring the infant receives the necessary building blocks for growth and development. This enhances the overall nutritional benefit of the feeding.
In summary, the connection between digestive symptom relief and these specialized formulas is direct and significant. By eliminating lactose as a potential trigger for digestive distress, these formulas facilitate improved comfort, digestion, and nutrient absorption, ultimately contributing to the health and well-being of lactose-sensitive infants. While providing symptom relief, proper assessment and guidance from a healthcare professional is still needed.
2. Alternative Carbohydrates Source
The absence of lactose necessitates the incorporation of alternative carbohydrate sources in lactose-free infant formula. This substitution is not merely a replacement but a critical element in ensuring the nutritional adequacy and digestive compatibility of the formula. The choice of carbohydrate significantly influences the formula’s digestibility, sweetness, and impact on blood glucose levels. Common alternatives include corn syrup solids, sucrose, glucose, and maltodextrin. Each source possesses distinct properties affecting infant metabolism and digestive processes. For example, corn syrup solids, a widely used option, provide a readily available source of glucose, supporting energy needs. Sucrose, another alternative, offers a similar energy profile but with a different metabolic pathway. Understanding the characteristics of these alternative carbohydrates is crucial for healthcare professionals and caregivers in selecting the most appropriate formula for an infant’s specific needs.
The selection of alternative carbohydrates directly addresses the digestive challenges faced by lactose-intolerant infants. When lactose, a disaccharide, is not properly broken down in the small intestine due to lactase deficiency, it can lead to fermentation by gut bacteria, resulting in gas, bloating, and diarrhea. Substituting lactose with monosaccharides or readily digestible polysaccharides bypasses this enzymatic requirement, mitigating digestive distress. Furthermore, the composition of the alternative carbohydrate blend can influence the gut microbiome. Some alternatives may promote the growth of beneficial bacteria, contributing to overall gut health. Careful consideration of these factors is essential in optimizing infant nutrition and minimizing adverse effects.
In conclusion, the alternative carbohydrate source is an indispensable component of lactose-free infant formula, serving as a nutritional foundation while addressing the digestive limitations of lactose intolerance. Its selection requires a comprehensive understanding of its metabolic effects, digestive properties, and potential impact on gut health. Challenges remain in optimizing the carbohydrate blend to mimic the benefits of lactose in standard infant formulas while ensuring digestive comfort and nutritional completeness. Future research should focus on identifying novel carbohydrate sources with improved digestibility and prebiotic effects, further enhancing the efficacy of lactose-free infant formulas.
3. Nutritional Completeness Assurance
Nutritional completeness assurance constitutes a fundamental aspect of infant formula design, particularly in the context of lactose-free variants. Standard infant formulas are formulated to mimic the nutritional profile of breast milk, providing essential macronutrients (proteins, fats, carbohydrates) and micronutrients (vitamins, minerals) required for optimal growth and development during infancy. When lactose, a primary carbohydrate source in breast milk and standard formulas, is removed due to lactose intolerance or sensitivity, it becomes imperative to ensure that the resulting lactose-free formulation continues to provide a nutritionally equivalent and balanced alternative. Failure to achieve nutritional completeness can lead to deficiencies, impacting growth trajectory, cognitive development, and immune function. The formulation must compensate for the removal of lactose with alternative carbohydrate sources while maintaining appropriate levels of all other essential nutrients. Regulatory standards, such as those set by the Food and Drug Administration (FDA) in the United States and similar bodies internationally, mandate that infant formulas meet specific nutritional requirements to safeguard infant health. For example, a lactose-free formula must still provide adequate levels of vitamins A, D, E, and K, as well as essential minerals like calcium, iron, and zinc, to support bone development, immune function, and overall physiological processes.
The challenges in achieving nutritional completeness in these formulas extend beyond merely replacing lactose with another carbohydrate. The bioavailability of nutrients, the digestibility of proteins and fats, and the potential interactions between ingredients must all be carefully considered. For instance, some alternative carbohydrate sources may affect the absorption of certain minerals. Similarly, changes in protein composition or fat blends can impact digestion and nutrient utilization. Therefore, the formulation process involves rigorous testing and analysis to ensure that the formula not only meets minimum regulatory requirements but also supports optimal nutrient absorption and utilization. Real-life examples of infants who have thrived on lactose-free formulas that have been carefully formulated for nutritional completeness underscore the practical significance of this principle. Conversely, cases where infants have experienced growth faltering or nutrient deficiencies due to inadequately formulated lactose-free formulas highlight the potential consequences of compromising nutritional completeness.
In conclusion, nutritional completeness assurance is not simply a desirable attribute but a non-negotiable imperative in the context of lactose-free infant formulas. It requires a comprehensive understanding of infant nutritional needs, a meticulous approach to formulation and testing, and adherence to stringent regulatory standards. While addressing the specific digestive challenges of lactose intolerance or sensitivity, the primary goal remains to provide an infant formula that supports optimal growth, development, and overall health. Future advancements in infant formula technology should continue to prioritize nutritional completeness, ensuring that all infants, regardless of their dietary needs, receive the nutrients necessary to thrive. The responsibility falls upon manufacturers, healthcare professionals, and regulatory bodies to collaborate in upholding these standards and safeguarding the health of the most vulnerable population.
4. Hydrolyzed Protein Option
The utilization of hydrolyzed protein represents a significant modification in infant formula formulation, frequently considered in conjunction with lactose-free preparations. This adaptation addresses digestive sensitivities that extend beyond lactose intolerance, targeting protein molecules that may trigger adverse reactions in some infants. The following points elaborate on the role and implications of hydrolyzed protein in this context.
- Reduced Allergenicity
Hydrolyzed protein formulas undergo a process where proteins are broken down into smaller peptide fragments. This reduces their allergenic potential, making them less likely to trigger an immune response in infants with cow’s milk protein allergy (CMPA) or sensitivity. In the context of lactose-free formulas, hydrolyzed proteins offer a dual benefit: addressing lactose intolerance while mitigating potential protein-related sensitivities. For example, an infant exhibiting persistent digestive distress despite lactose removal may benefit from a formula with both lactose-free and hydrolyzed protein characteristics.
- Improved Digestibility
The smaller peptide size in hydrolyzed protein formulas enhances their digestibility. Infants with immature or compromised digestive systems may find it easier to break down and absorb hydrolyzed proteins compared to intact proteins. This improved digestibility can reduce symptoms such as gas, bloating, and abdominal discomfort. The combination of lactose removal and protein hydrolysis can synergistically alleviate digestive burden, promoting enhanced nutrient absorption and overall comfort. An infant struggling with both lactose and protein digestion would likely experience improved tolerance with this option.
- Types of Hydrolyzed Protein Formulas
There are varying degrees of protein hydrolysis, ranging from partially hydrolyzed to extensively hydrolyzed formulas. Extensively hydrolyzed formulas, where proteins are broken down into the smallest peptide fragments and even amino acids, are typically recommended for infants with confirmed CMPA or severe protein sensitivity. Partially hydrolyzed formulas may be suitable for infants with milder sensitivities or as a preventative measure. The choice of hydrolysis level depends on the severity of the infant’s symptoms and the recommendations of a healthcare professional. When selecting a lactose-free formula, caregivers should consider the degree of protein hydrolysis in relation to the infant’s specific needs.
- Clinical Applications and Considerations
The decision to use a lactose-free, hydrolyzed protein formula should be made in consultation with a pediatrician or other qualified healthcare provider. These formulas are generally more expensive than standard formulas, and their use should be based on a clear clinical indication. While they can provide significant relief for infants with specific digestive issues, they are not necessarily superior to standard formulas for infants without such conditions. Caregivers should be aware of potential changes in stool consistency and odor associated with hydrolyzed protein formulas. In cases of suspected CMPA, diagnostic testing may be necessary to confirm the diagnosis and guide formula selection.
The integration of hydrolyzed protein into lactose-free infant formulas represents a targeted approach to addressing complex digestive sensitivities in infants. By reducing allergenicity and improving digestibility, these formulations can offer substantial relief to infants who experience persistent discomfort with standard formulas. However, the selection of a lactose-free, hydrolyzed protein formula should always be guided by the recommendations of a healthcare professional, based on a thorough assessment of the infant’s individual needs and clinical presentation.
5. Healthcare Professional Guidance
Healthcare professional guidance serves as a critical pillar in the appropriate selection and utilization of lactose-free infant formula. Due to the potential for misdiagnosis, inappropriate formula selection, and the importance of ensuring adequate nutritional intake, consultation with qualified healthcare providers is paramount. The complexities of infant digestive health necessitate expert evaluation and tailored recommendations.
- Diagnostic Accuracy and Differential Diagnosis
Gastrointestinal symptoms in infants, such as fussiness, gas, diarrhea, and vomiting, can stem from various underlying causes. Healthcare professionals possess the expertise to differentiate lactose intolerance or sensitivity from other conditions, including cow’s milk protein allergy, infections, or anatomical abnormalities. A misdiagnosis can lead to unnecessary dietary restrictions or delays in appropriate treatment. Diagnostic tools, such as stool tests or elimination diets, may be employed to confirm lactose intolerance. Moreover, healthcare professionals can assess the severity of lactose intolerance and determine whether a lactose-free formula is truly warranted. An example involves an infant presenting with persistent diarrhea; a healthcare professional would rule out infectious causes and assess for other dietary sensitivities before recommending a lactose-free formula.
- Formula Selection Tailoring
The market offers a variety of lactose-free infant formulas, each with distinct compositions and potential benefits. Healthcare professionals can guide parents in selecting the most appropriate formula based on the infant’s specific needs and clinical presentation. Factors to consider include the source of alternative carbohydrates, the presence of hydrolyzed proteins, and the overall nutritional profile. For instance, an infant with a family history of allergies may benefit from a lactose-free formula containing partially hydrolyzed proteins to reduce the risk of allergic reactions. Similarly, an infant with severe lactose intolerance may require a formula with a readily digestible carbohydrate source. Healthcare professionals can also advise on appropriate transition strategies when switching formulas, minimizing the risk of digestive upset. The guidance ensures that the chosen formula aligns with the infants physiological requirements.
- Nutritional Adequacy and Growth Monitoring
Lactose provides a significant source of calories and carbohydrates in standard infant formulas. When lactose is removed, it is essential to ensure that the lactose-free formula provides adequate alternative sources of energy and nutrients to support optimal growth and development. Healthcare professionals can monitor the infant’s growth trajectory, weight gain, and overall nutritional status to ensure that the formula is meeting their needs. They can also provide guidance on appropriate feeding volumes and frequencies. If an infant experiences growth faltering or nutrient deficiencies while on a lactose-free formula, the healthcare professional can adjust the feeding plan or recommend alternative formulas. The monitoring guarantees adequate nutrition, despite dietary modifications.
- Management of Complications and Associated Conditions
Infants with lactose intolerance may also have other co-existing medical conditions or develop complications. Healthcare professionals are equipped to manage these situations effectively. For example, an infant with lactose intolerance may also have reflux or colic. The healthcare professional can provide guidance on appropriate positioning techniques, feeding strategies, and, if necessary, medications to manage these conditions. They can also monitor for potential complications, such as dehydration or electrolyte imbalances, and provide prompt treatment. Effective management can provide comprehensive care for the infant’s well-being.
In conclusion, healthcare professional guidance represents an indispensable component in the successful use of lactose-free infant formula. From accurate diagnosis and tailored formula selection to nutritional monitoring and the management of associated conditions, the expertise of healthcare providers ensures that infants receive the appropriate care and support to thrive. The considerations provide clarity and direction for parents navigating the complexities of infant nutrition and digestive health. Without professional guidance, infants may face misdiagnosis, inappropriate dietary interventions, and suboptimal health outcomes.
6. Gradual Transition Important
The significance of a gradual transition to lactose-free infant formula lies in minimizing digestive upset and facilitating adaptation to the altered composition. Abrupt changes can disrupt the delicate balance of the infant’s gastrointestinal system, leading to adverse reactions and hindering the acceptance of the new formula.
- Minimizing Digestive Discomfort
The abrupt introduction of a completely new formula composition can overwhelm an infant’s digestive system, potentially causing gas, bloating, diarrhea, or constipation. A gradual transition allows the gut microbiome to adjust to the new carbohydrate source and protein structure, mitigating these discomforts. For example, slowly increasing the proportion of lactose-free formula over several days enables the digestive enzymes to adapt, reducing the likelihood of digestive distress.
- Facilitating Acceptance of New Taste and Texture
Lactose-free formulas often differ in taste and texture compared to standard formulas. An abrupt switch may lead to rejection due to unfamiliarity. A gradual introduction allows the infant to acclimate to the new sensory experience, increasing acceptance and ensuring adequate intake. Consider a scenario where an infant accustomed to the sweet taste of lactose-containing formula may initially refuse a lactose-free version; a gradual blending of the two formulas can bridge this gap.
- Assessing Tolerance and Identifying Sensitivities
A gradual transition allows caregivers to closely monitor the infant’s response to the new formula, identifying any potential sensitivities or adverse reactions. Abrupt changes can make it difficult to pinpoint the cause of any issues that arise. By slowly increasing the proportion of lactose-free formula, caregivers can readily observe changes in stool patterns, skin condition, and behavior, enabling timely intervention if necessary. For example, a gradual transition may reveal a sensitivity to a specific ingredient in the lactose-free formula, prompting a switch to an alternative brand.
- Maintaining Adequate Nutrient Intake
During the transition period, it is crucial to ensure that the infant continues to receive adequate nutrients. An abrupt switch to lactose-free formula without careful monitoring can lead to inadequate caloric intake or nutrient deficiencies. A gradual transition allows caregivers to track the infant’s feeding habits and adjust the feeding plan as needed, ensuring that their nutritional needs are met. For instance, if an infant initially consumes less lactose-free formula, the proportion of standard formula can be adjusted to maintain adequate caloric intake during the transition.
The facets of gradual transition contribute to the overall success of utilizing lactose-free infant formula. By minimizing digestive distress, facilitating acceptance, assessing tolerance, and maintaining nutrient intake, this approach promotes the infant’s well-being and ensures a smooth adaptation to the altered dietary composition. Real-world examples highlight that a controlled transition yields higher acceptance rates and improved digestive outcomes, ultimately benefiting both the infant and the caregivers.
7. Ingredient List Review
For lactose-free infant formula, meticulous review of the ingredient list serves as a critical safeguard against unintended exposure to allergens and ensures the formula’s suitability for the infant’s specific dietary needs. While the primary intention is to eliminate lactose, ingredient lists reveal the composition of alternative carbohydrates, protein sources, and added nutrients. These components can trigger adverse reactions in sensitive infants, necessitating careful scrutiny. For instance, a lactose-free formula may utilize corn syrup solids as a carbohydrate source. An infant sensitive to corn could experience digestive distress, despite the absence of lactose. Therefore, the absence of lactose alone does not guarantee a hypoallergenic or universally tolerated product. Ingredient list review allows caregivers and healthcare professionals to identify potential allergens, such as soy, whey, or hydrolyzed proteins, which may be present even in lactose-free formulations. The practical significance lies in preventing allergic reactions, digestive upset, and other adverse effects that can compromise the infant’s health and well-being.
The process of ingredient list review extends beyond identifying allergens. It also enables assessment of the nutritional completeness and quality of the formula. The order in which ingredients are listed reflects their proportion in the product; a higher-ranking ingredient is present in greater quantity. Analyzing the order provides insight into the primary carbohydrate source and the relative abundance of essential nutrients. Furthermore, ingredient lists reveal the presence of additives, preservatives, and artificial flavors. Some infants may exhibit sensitivity to these substances, warranting selection of formulas with minimal additives. A real-world example involves comparing two lactose-free formulas; one may contain a higher concentration of added sugars, potentially contributing to increased fussiness or dental caries. By comparing ingredient lists, caregivers can make informed decisions aligning with their infant’s specific nutritional requirements and preferences.
In conclusion, thorough ingredient list review represents an indispensable component of responsible lactose-free infant formula selection. It serves as a proactive measure to prevent allergic reactions, ensure nutritional adequacy, and minimize exposure to potentially harmful additives. While healthcare professionals provide essential guidance, caregivers must actively engage in ingredient list review to make informed decisions aligned with their infant’s individual needs. Ongoing awareness and critical evaluation of ingredient lists remain essential for optimizing infant health and well-being. The challenge lies in navigating complex ingredient terminology and understanding the potential effects of various components, necessitating continued education and resource accessibility for caregivers.
Frequently Asked Questions About Lactose Free Baby Formula
The subsequent section addresses common inquiries regarding lactose-free infant formula, providing clarity on its use, benefits, and potential considerations.
Question 1: What distinguishes lactose-free infant formula from standard infant formula?
The primary distinction lies in the absence of lactose, a naturally occurring sugar found in milk. Standard formulas contain lactose, whereas lactose-free versions utilize alternative carbohydrates, such as corn syrup solids or sucrose, to provide energy.
Question 2: When is it appropriate to consider lactose-free infant formula?
This type of formula is generally considered for infants exhibiting symptoms suggestive of lactose intolerance or sensitivity. These symptoms may include gas, bloating, diarrhea, fussiness, or abdominal discomfort following feeding. A healthcare professional’s assessment is essential to confirm the diagnosis and determine if a lactose-free formula is warranted.
Question 3: Does lactose-free infant formula provide complete nutrition?
Reputable lactose-free formulas are designed to provide complete and balanced nutrition, mirroring the nutritional profile of standard infant formulas and breast milk. They contain essential proteins, fats, carbohydrates, vitamins, and minerals necessary for infant growth and development. Careful selection of a reputable brand and adherence to preparation instructions are crucial to ensure adequate nutrient intake.
Question 4: Are there potential drawbacks to using lactose-free infant formula?
While generally safe and effective, lactose-free formulas may not be necessary for all infants. In some cases, symptoms attributed to lactose intolerance may stem from other underlying causes. Furthermore, some lactose-free formulas may have a different taste or texture, which may affect infant acceptance. It is crucial to consult with a healthcare professional to determine if the benefits outweigh any potential drawbacks in a particular situation.
Question 5: How should the transition to lactose-free infant formula be managed?
A gradual transition is generally recommended to minimize digestive upset. Mixing increasing amounts of the lactose-free formula with the existing formula over several days allows the infant’s digestive system to adapt. Close monitoring for any changes in stool patterns, behavior, or overall well-being is essential during the transition period.
Question 6: Can lactose intolerance be a permanent condition in infants?
In most cases, lactose intolerance in infants is temporary and related to the immaturity of the digestive system. Many infants outgrow lactose intolerance by the time they reach toddlerhood. However, in rare instances, congenital lactose intolerance may be present, requiring long-term dietary management.
The information provided in these frequently asked questions aims to offer general guidance. Individual circumstances may vary, and professional medical advice should always be sought for specific health concerns.
The next section will summarize the key considerations and offer concluding remarks on lactose-free infant formula usage.
Conclusion
This exploration of lactose free baby formula has underscored its crucial role in addressing the nutritional needs of infants with lactose sensitivities. The discussion has encompassed the formula’s composition, benefits, potential drawbacks, and the importance of healthcare professional guidance in its selection and use. Key considerations include accurate diagnosis of lactose intolerance, appropriate formula selection based on individual needs, gradual transition strategies, and ongoing monitoring of nutritional status.
Given the complexities of infant digestive health and the potential for varied responses to dietary interventions, informed decision-making is paramount. Continued research and advancements in infant formula technology are essential to optimize the safety and efficacy of lactose free baby formula, ensuring that all infants receive the necessary nutrients for healthy growth and development. Prioritizing infant well-being remains the central objective in the ongoing evolution of infant nutrition practices.