Infant nutrition products designed without lactose are specialized formulas tailored for babies who experience difficulty digesting lactose, a sugar naturally found in milk. These formulations substitute lactose with alternative carbohydrates, such as corn syrup solids or sucrose, to provide a readily digestible energy source. One common example involves infants diagnosed with lactose intolerance or galactosemia who require such dietary modifications to prevent gastrointestinal distress.
These specialized formulas offer a crucial nutritional alternative for infants unable to tolerate standard milk-based products. The primary benefit lies in mitigating symptoms like gas, bloating, diarrhea, and abdominal pain often associated with lactose intolerance. Historically, the development of lactose-free options significantly improved the health outcomes for affected infants, ensuring they receive adequate nutrition without experiencing adverse reactions. This advancement has had a profound impact on infant feeding practices worldwide.
The following sections will explore the specific ingredients and nutritional composition of these specialized formulas, delve into the medical conditions necessitating their use, and compare them to other available infant formula options. Furthermore, we will examine the regulatory guidelines governing their production and distribution, providing a comprehensive understanding of their role in infant nutrition.
Guidance on Utilizing Lactose-Free Infant Formula
This section provides essential guidelines for the appropriate and effective utilization of lactose-free infant formula. Strict adherence to these recommendations ensures optimal infant health and minimizes potential complications.
Tip 1: Consult a Pediatrician: Prior to initiating lactose-free infant formula, a thorough medical evaluation by a qualified pediatrician is imperative. Professional guidance ensures the necessity and suitability of this specialized formula for the individual infant’s needs.
Tip 2: Adhere to Preparation Instructions: Precise adherence to the manufacturer’s preparation instructions is crucial. Incorrect mixing ratios may compromise nutritional content or lead to digestive issues. Use the provided measuring scoop and follow water-to-powder ratios meticulously.
Tip 3: Monitor Infant Response: Closely observe the infant’s reaction to the formula. Changes in stool consistency, frequency, or signs of discomfort should be promptly reported to a healthcare provider. This proactive monitoring facilitates timely adjustments to the feeding plan.
Tip 4: Ensure Adequate Nutritional Intake: Confirm that the chosen lactose-free formula provides all essential nutrients required for optimal growth and development. Compare the nutritional profile to standard infant formula and consult with a pediatrician or registered dietitian if concerns arise.
Tip 5: Practice Proper Hygiene: Stringent hygiene practices during formula preparation are essential to prevent bacterial contamination. Sterilize bottles, nipples, and mixing equipment regularly. Always wash hands thoroughly before handling formula and feeding supplies.
Tip 6: Avoid Overfeeding: Follow recommended feeding guidelines based on the infant’s age and weight. Overfeeding can lead to discomfort and potential health complications. Consult a pediatrician for personalized feeding recommendations.
Effective implementation of these guidelines contributes significantly to the well-being of infants requiring lactose-free formula. By following professional advice and diligently monitoring the infant’s response, caregivers can ensure optimal nutritional support and minimize adverse effects.
The following sections will address specific considerations related to transitioning to and from lactose-free formula, as well as potential long-term implications for infant health.
1. Suitable Alternative
The term “suitable alternative” in the context of lactose-free infant formula signifies its role as a nutritionally appropriate replacement for standard, lactose-containing formulas. Its suitability is predicated on the infant’s inability to properly digest lactose, a disaccharide sugar present in mammalian milk. The following aspects delineate its function and characteristics:
- Gastrointestinal Symptom Management
Lactose intolerance, whether primary or secondary, manifests through digestive symptoms such as diarrhea, gas, bloating, and abdominal discomfort. Lactose-free infant formulas effectively mitigate these symptoms by removing the causative agent, lactose, thereby providing relief and promoting intestinal comfort. Real-world examples include infants diagnosed with transient lactose intolerance following a bout of gastroenteritis, where a temporary switch to a lactose-free formula resolves the digestive distress.
- Nutritional Equivalence
A crucial aspect of a suitable alternative is its ability to provide equivalent nutritional value to standard formulas. Lactose-free formulas are designed to meet or exceed established nutritional guidelines, ensuring that infants receive adequate amounts of proteins, fats, carbohydrates (using alternative sources like corn syrup solids or sucrose), vitamins, and minerals essential for growth and development. Regular monitoring of the infant’s growth parameters ensures the formula is adequately meeting their nutritional needs.
- Specialized Medical Conditions
Beyond lactose intolerance, specific medical conditions necessitate the use of lactose-free formulas. Galactosemia, a rare genetic metabolic disorder, prevents the body from processing galactose, a component of lactose. In such cases, a completely lactose-free and galactose-free formula is a medical necessity. The use of these formulas is critical in preventing serious complications associated with galactosemia, such as liver damage and developmental delays.
- Temporary Dietary Intervention
Lactose-free infant formula can serve as a temporary dietary intervention for infants experiencing digestive issues following antibiotic treatment, which can disrupt the intestinal flora and induce transient lactose intolerance. The temporary switch allows the gut to heal and repopulate with beneficial bacteria, after which a gradual reintroduction of standard formula may be considered under medical supervision. This temporary use highlights the adaptable nature of lactose-free formula in addressing specific and transient digestive challenges.
In summation, the “suitable alternative” descriptor accurately reflects the role of lactose-free infant formula as a vital dietary option for infants with lactose intolerance, galactosemia, or other conditions necessitating lactose avoidance. Its ability to provide symptomatic relief, nutritional equivalence, and address specific medical needs underscores its importance in ensuring optimal infant health and development.
2. Digestive Symptom Alleviation
Digestive symptom alleviation constitutes a primary consideration in the utilization of lactose-free infant formula. The reduction or elimination of gastrointestinal distress forms a central rationale for selecting this specialized nutritional product for infants experiencing lactose intolerance or related conditions.
- Reduction of Diarrhea
Diarrhea, characterized by frequent and watery bowel movements, represents a common manifestation of lactose intolerance in infants. Undigested lactose in the intestinal tract draws water into the colon, leading to increased stool volume and frequency. Lactose-free infant formula mitigates this process by eliminating lactose, thereby reducing osmotic pressure and decreasing the incidence of diarrheal episodes. Clinical observations consistently demonstrate a decrease in stool frequency and improved stool consistency following the introduction of lactose-free formula in lactose-intolerant infants. This reduction is particularly significant in preventing dehydration and promoting overall fluid balance.
- Diminished Flatulence and Bloating
Intestinal gas production, resulting in flatulence and abdominal bloating, frequently accompanies lactose malabsorption. Undigested lactose serves as a substrate for bacterial fermentation in the colon, producing gases such as hydrogen, methane, and carbon dioxide. Lactose-free infant formula eliminates this fermentation process, leading to a substantial reduction in gas production and associated discomfort. Clinical assessments often reveal a noticeable decrease in infant irritability and abdominal distension following the adoption of a lactose-free feeding regimen. This improvement contributes to enhanced infant comfort and improved sleep patterns.
- Alleviation of Abdominal Pain and Cramping
Abdominal pain and cramping, often described as colic-like symptoms, can result from the presence of undigested lactose in the intestinal tract. Bacterial fermentation and the resulting distension of the intestinal wall trigger visceral pain receptors, leading to discomfort and crying episodes. Lactose-free infant formula addresses this issue by preventing lactose accumulation, thereby reducing intestinal distension and minimizing pain signals. Caregiver reports frequently document a decrease in crying duration and an overall reduction in signs of abdominal discomfort following the implementation of lactose-free feeding practices. This alleviation of pain symptoms improves the infant’s overall well-being and reduces parental stress.
- Improved Nutrient Absorption
While lactose intolerance primarily affects carbohydrate digestion, persistent diarrhea and inflammation associated with lactose malabsorption can indirectly impair the absorption of other essential nutrients. By resolving the underlying cause of digestive distress, lactose-free infant formula promotes improved absorption of fats, proteins, vitamins, and minerals. Studies indicate that infants receiving lactose-free formula demonstrate enhanced weight gain and growth parameters compared to those consuming lactose-containing formulas while experiencing ongoing malabsorption. This improvement in nutrient absorption supports optimal development and long-term health outcomes.
Collectively, these facets underscore the significance of digestive symptom alleviation in guiding the appropriate application of lactose-free infant formula. The ability to effectively manage diarrhea, flatulence, abdominal pain, and promote nutrient absorption highlights the therapeutic value of this specialized formula for infants with diagnosed or suspected lactose intolerance.
3. Nutritional Adequacy
Nutritional adequacy in the context of lactose-free infant formula is of paramount importance. It underscores the requirement that these specialized formulas must provide a complete and balanced nutritional profile comparable to standard, lactose-containing formulas, ensuring optimal growth and development in infants who cannot tolerate lactose.
- Macronutrient Composition
Lactose-free formulas must supply adequate quantities of protein, fat, and carbohydrates to meet the infant’s energy needs and support tissue synthesis. Protein sources are typically derived from soy, extensively hydrolyzed casein, or amino acids. Fat blends often include vegetable oils such as soy, sunflower, or coconut oil to provide essential fatty acids like linoleic and alpha-linolenic acids. Carbohydrates, replacing lactose, frequently consist of corn syrup solids, sucrose, or glucose polymers. The precise ratios and types of macronutrients are carefully formulated to mimic the composition of human milk and standard formulas, supporting optimal growth rates. Examples include the formulation of hypoallergenic formulas for infants with cow’s milk protein allergy, where extensively hydrolyzed proteins are combined with lactose-free carbohydrates and appropriate fat blends to ensure both tolerance and nutritional completeness.
- Micronutrient Fortification
Adequate micronutrient content is critical in lactose-free infant formulas to prevent deficiencies and support various physiological functions. These formulas are typically fortified with vitamins (A, D, E, K, C, B-complex), minerals (calcium, phosphorus, iron, zinc, iodine), and trace elements (copper, manganese, selenium). The levels of fortification are established based on recommended daily intakes for infants and are adjusted to account for potential differences in bioavailability due to the absence of lactose. For instance, iron fortification is crucial to prevent iron deficiency anemia, while vitamin D supplementation supports calcium absorption and bone mineralization. Regulatory agencies mandate specific fortification levels to ensure that lactose-free formulas meet defined nutritional standards.
- Bioavailability Considerations
The bioavailability of nutrients in lactose-free formulas is a significant factor in assessing nutritional adequacy. The absence of lactose can affect the absorption of certain minerals, such as calcium. Manufacturers often incorporate strategies to enhance bioavailability, such as using specific forms of minerals or adjusting the pH of the formula to promote absorption. For example, some lactose-free formulas include prebiotics or probiotics to support a healthy gut microbiome, which can improve nutrient absorption. Clinical studies are frequently conducted to assess the bioavailability of key nutrients in these formulas, providing evidence of their nutritional efficacy.
- Meeting Growth and Developmental Milestones
The ultimate measure of nutritional adequacy in lactose-free infant formula is the infant’s ability to achieve appropriate growth and developmental milestones. Regular monitoring of weight, length, and head circumference, along with assessments of motor and cognitive development, provides valuable insights into the formula’s effectiveness. Infants consuming lactose-free formulas should exhibit growth patterns comparable to those consuming standard formulas, indicating that their nutritional needs are being adequately met. Healthcare providers routinely track these parameters to ensure that infants are thriving on their chosen formula and to identify any potential nutritional deficiencies early on.
These facets collectively emphasize the stringent requirements for nutritional adequacy in lactose-free infant formulas. By ensuring appropriate macronutrient composition, micronutrient fortification, bioavailability, and monitoring growth parameters, these specialized formulas can effectively support the health and development of infants who cannot tolerate lactose, providing a nutritionally complete alternative to standard formulas.
4. Medical Necessity
The designation of “medical necessity” in the context of lactose-free infant formula underscores specific clinical conditions wherein the utilization of such formulas is not merely preferential but essential for the infant’s health and well-being. These conditions necessitate the elimination of lactose from the infant’s diet to prevent or mitigate adverse health outcomes.
- Confirmed Lactose Intolerance
Infants diagnosed with lactose intolerance, either congenital or acquired, require lactose-free formulas to avoid gastrointestinal distress. Congenital lactose intolerance, a rare genetic condition, presents from birth, necessitating immediate lactose elimination. Acquired lactose intolerance, often following gastroenteritis, results in temporary lactase enzyme deficiency. In both scenarios, lactose-free formulas mitigate symptoms like diarrhea, abdominal pain, and bloating, preventing dehydration and malnutrition. Diagnostic confirmation via lactose tolerance tests or stool analysis substantiates this medical necessity.
- Galactosemia
Galactosemia, a rare inherited metabolic disorder, renders infants unable to process galactose, a monosaccharide component of lactose. Lactose-free formulas are indispensable in this condition, as lactose breakdown would lead to galactose accumulation, causing liver damage, developmental delays, and even death. Galactosemia screening at birth detects this condition, mandating immediate dietary intervention with lactose-free and galactose-free formulas. Strict adherence to this dietary regimen is crucial for preventing long-term complications.
- Post-Surgical or Severe Gastrointestinal Conditions
Following certain surgical procedures or in cases of severe gastrointestinal illnesses, infants may experience transient lactase deficiency or impaired intestinal absorption. Conditions such as necrotizing enterocolitis (NEC) or extensive bowel resection can compromise lactase production and intestinal integrity. Lactose-free formulas provide a readily digestible nutritional source, reducing osmotic load and minimizing intestinal irritation during the recovery phase. The duration of lactose-free feeding is determined by the resolution of the underlying condition and the restoration of normal intestinal function.
- Cow’s Milk Protein Allergy (CMPA) with Secondary Lactose Intolerance
Some infants with CMPA may develop secondary lactose intolerance due to intestinal inflammation and damage caused by the allergic reaction. In such cases, a formula that is both lactose-free and hypoallergenic (extensively hydrolyzed or amino acid-based) is medically necessary. The dual elimination addresses both the allergic trigger (cow’s milk protein) and the resulting lactose malabsorption, alleviating symptoms and promoting intestinal healing. Diagnosis of CMPA often involves allergy testing and clinical assessment of symptom improvement with hypoallergenic formulas.
These conditions exemplify scenarios where lactose-free infant formula transcends a mere dietary preference and becomes a crucial medical intervention. Proper diagnosis, informed clinical decision-making, and diligent monitoring are essential to ensure that infants receive the appropriate nutritional support tailored to their specific medical needs.
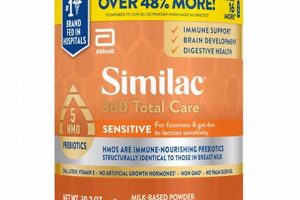
5. Formula Ingredients
The composition of lactose-free infant formula necessitates a detailed examination of its ingredients. The absence of lactose, the primary carbohydrate in standard formulas, requires the substitution of alternative carbohydrates to provide adequate energy for the infant. Common substitutes include corn syrup solids, sucrose, or glucose polymers. The selection of these carbohydrates influences the formula’s osmolality and digestibility. Furthermore, the protein source in lactose-free formulas often differs from standard cow’s milk-based formulas, frequently utilizing soy protein isolate, hydrolyzed casein, or, in cases of severe allergies, amino acids. The choice of protein source affects allergenicity and amino acid profile, demanding careful consideration to meet the infant’s nutritional requirements. The fat component typically consists of a blend of vegetable oils, providing essential fatty acids necessary for brain development and overall growth. The specific blend aims to replicate the fatty acid profile of breast milk as closely as possible. Finally, fortification with vitamins and minerals is crucial to ensure nutritional completeness, compensating for any potential differences in bioavailability compared to standard formulas. For instance, the presence of phytates in soy-based formulas can affect mineral absorption, necessitating adjusted fortification levels.
Understanding the specific ingredients within lactose-free infant formula is essential for healthcare professionals and caregivers alike. The careful selection and processing of these ingredients directly influence the formula’s suitability for infants with lactose intolerance or other medical conditions requiring lactose avoidance. For example, extensively hydrolyzed protein formulas are often used for infants with cow’s milk protein allergy, where the protein molecules are broken down to reduce their allergenicity. The carbohydrate source in these formulas must also be lactose-free to address both conditions concurrently. The addition of prebiotics or probiotics in some formulas aims to promote a healthy gut microbiome, potentially improving digestion and reducing the risk of infections. Monitoring the ingredient list for potential allergens or sensitivities is also a critical aspect of responsible formula selection.
In summary, the effectiveness and safety of lactose-free infant formula hinge on the careful selection, processing, and balancing of its constituent ingredients. The substitution of lactose with alternative carbohydrates, the choice of protein source, the fat blend composition, and micronutrient fortification all contribute to the formula’s nutritional adequacy and tolerability. Awareness of these components enables informed decision-making in selecting the most appropriate formula for individual infants, addressing specific dietary needs and medical conditions while ensuring optimal growth and development.
Frequently Asked Questions About Lactose-Free Infant Formula
The following questions address common concerns and misconceptions regarding lactose-free infant formula. The information provided aims to offer clarity and guidance for caregivers and healthcare professionals.
Question 1: What defines a lactose-free infant formula?
A lactose-free infant formula is characterized by the complete absence of lactose, a disaccharide sugar naturally found in mammalian milk. Alternative carbohydrate sources, such as corn syrup solids or sucrose, replace lactose to provide energy.
Question 2: Under what medical conditions is lactose-free infant formula necessary?
Lactose-free infant formula is medically necessary for infants diagnosed with lactose intolerance (congenital or acquired) and galactosemia. It may also be indicated in cases of transient lactase deficiency following surgery or severe gastrointestinal infections.
Question 3: Does lactose-free infant formula provide the same nutritional value as standard formulas?
Reputable lactose-free infant formulas are designed to provide comparable nutritional value to standard, lactose-containing formulas. They are fortified with essential vitamins, minerals, and macronutrients to support optimal growth and development.
Question 4: How does one determine if an infant requires lactose-free infant formula?
The decision to use lactose-free infant formula should be made in consultation with a pediatrician. Symptoms such as persistent diarrhea, abdominal bloating, and excessive gas, particularly after feeding, may indicate lactose intolerance, warranting further investigation.
Question 5: Are there potential risks associated with the long-term use of lactose-free infant formula?
When used appropriately and under medical supervision, lactose-free infant formula is generally safe for long-term use. However, it is crucial to ensure that the chosen formula provides adequate nutrition and that the infant’s growth and development are monitored regularly.
Question 6: Can an infant transition back to standard formula after using lactose-free infant formula?
The possibility of transitioning back to standard formula depends on the underlying cause of lactose intolerance. In cases of transient lactase deficiency, a gradual reintroduction of lactose-containing formula may be attempted under medical guidance. Congenital lactose intolerance or galactosemia typically require lifelong adherence to lactose-free diets.
The information provided herein is intended for general knowledge and should not substitute professional medical advice. Consultation with a healthcare provider is essential for personalized guidance and management of infant feeding.
The following section will address practical considerations related to preparing and storing lactose-free infant formula.
Conclusion
This article has comprehensively explored the intricacies of lactose-free baby formula, emphasizing its role as a critical nutritional intervention for infants unable to digest lactose. Key considerations, including nutritional adequacy, medical necessity, and the importance of ingredient selection, have been thoroughly examined. Understanding these aspects is paramount for informed decision-making by healthcare professionals and caregivers alike.
The appropriate use of lactose baby formula ensures that infants with specific medical needs receive the necessary nutrients for healthy growth and development. Continued research and vigilance in formula formulation and usage remain essential to optimize infant health outcomes and address potential long-term implications.