An appliance designed to automate the preparation of infant nutrition is the subject of this discussion. These devices typically measure, mix, and heat water and formula powder to create a bottle of consistent temperature and concentration. The goal is to streamline and standardize the process of feeding infants with prepared formula.
Automated formula preparation offers potential advantages, including time savings and reduced risk of error in measurements. Historically, parents and caregivers have relied on manual methods, which can be prone to inconsistencies. Modern conveniences aim to alleviate these challenges, ensuring a reliably prepared bottle at each feeding. This contributes to both parental peace of mind and potentially more consistent nutrition for the infant.
The following sections will delve into the factors to consider when evaluating automated infant formula preparation devices, exploring aspects such as ease of use, cleaning requirements, safety features, and the types of formula compatible with each appliance. This exploration aims to provide a comprehensive overview of the current landscape of automated formula preparation technology.
Guidance on Automated Infant Formula Preparation
The following recommendations aim to provide a framework for the effective and safe utilization of automated infant formula preparation devices. Adherence to these guidelines can contribute to the well-being of the infant and the longevity of the appliance.
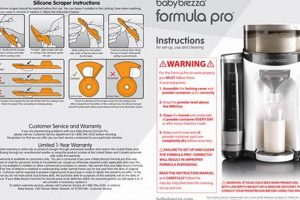
Tip 1: Prioritize Hygiene: Consistent cleaning of all device components is paramount. Follow the manufacturer’s instructions meticulously to prevent bacterial growth. Regular disassembly and washing, including the water tank, mixing components, and dispensing nozzle, are essential.
Tip 2: Verify Formula Compatibility: Not all formula types are suitable for every machine. Consult the device’s documentation and the formula manufacturer to confirm compatibility. Using incompatible formulas may result in clogs, inaccurate measurements, or damage to the appliance.
Tip 3: Utilize Purified Water: The quality of water significantly impacts infant health. Employ only purified or distilled water that meets recognized safety standards. Avoid tap water unless its safety and purity have been independently verified. This minimizes the risk of introducing contaminants.
Tip 4: Calibrate Accurately: Ensure the device is properly calibrated according to the formula’s concentration requirements. Incorrect calibration can lead to under- or over-concentration, which can negatively affect the infant’s nutritional intake. Use a calibrated scale if needed.
Tip 5: Monitor Dispensing Consistency: Regularly inspect dispensed formula for consistency in volume and texture. Note any variations in consistency and address the potential cause, such as formula clumping or machine malfunction.
Tip 6: Adhere to Expiration Dates: Always check the expiration dates on formula containers and water filters. Expired formula may have reduced nutritional value, and expired filters may lose their effectiveness.
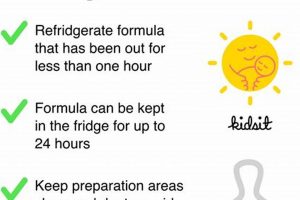
Tip 7: Follow Storage Protocols: Store formula and prepared bottles according to recommended guidelines to prevent bacterial growth. Discard any unused formula after the recommended timeframe to maintain freshness.
The diligent application of these tips ensures the safe and effective employment of automated infant formula preparation devices. Consistent attention to hygiene, compatibility, calibration, and storage protocols maximizes the benefits and minimizes potential risks.
The next phase of this discourse will explore common troubleshooting scenarios and offer solutions for resolving operational issues.
1. Hygiene
Hygiene represents a cornerstone of safe and effective infant formula preparation, particularly when utilizing automated devices. The maintenance of sanitary conditions within these machines directly impacts the health and well-being of the infant consuming the prepared formula. Neglecting hygienic practices can lead to bacterial contamination and subsequent health risks.
- Component Sterilization
Automated formula makers possess multiple components that come into direct contact with water and formula. Regular sterilization of these parts, including the water tank, mixing mechanisms, and dispensing nozzles, is crucial. For example, residual milk or formula particles can foster bacterial growth, potentially leading to gastrointestinal distress in infants. Sterilization methods typically involve boiling, steaming, or the use of specialized sanitizing solutions.
- Water Quality and Reservoir Maintenance
The water reservoir serves as a breeding ground for microorganisms if not properly maintained. Frequent emptying and cleaning of the reservoir are essential. The use of purified or distilled water minimizes the introduction of contaminants. For instance, tap water may contain minerals or bacteria that can proliferate within the reservoir, compromising the hygiene of the prepared formula.
- Formula Powder Handling
The formula powder itself can be a source of contamination if mishandled. Proper storage of the formula container and the use of a clean measuring scoop are vital. Exposure to moisture or unsanitary environments can introduce bacteria to the powder. For example, using a damp or unwashed scoop can transfer contaminants to the bulk formula supply.
- Cleaning Frequency and Procedures
The frequency of cleaning impacts the overall hygiene of the device. Manufacturers typically provide specific cleaning schedules and procedures. Adhering to these recommendations is crucial. Infrequent cleaning or improper techniques can result in the buildup of residue and the proliferation of harmful bacteria. For example, neglecting to disassemble and thoroughly clean the mixing components can lead to persistent contamination.
The interconnectedness of these hygienic practices highlights the importance of comprehensive sanitation protocols for automated formula preparation devices. Prioritizing cleanliness at every stage, from component sterilization to water quality and formula handling, ensures the safety and well-being of the infant. Neglecting any aspect of hygiene can compromise the entire process, undermining the benefits of automated preparation and potentially leading to adverse health outcomes.
2. Accuracy
In the context of automated infant formula preparation, accuracy denotes the device’s ability to consistently dispense precise quantities of water and formula powder. This precision directly influences the nutritional composition and safety of the prepared feed, rendering accuracy a paramount consideration.
- Formula-to-Water Ratio
The correct formula-to-water ratio is vital for providing the infant with appropriate caloric intake and nutrient levels. Deviations from the recommended ratio can lead to nutritional imbalances. For instance, overly concentrated formula may cause dehydration and electrolyte imbalances, while diluted formula may result in inadequate weight gain and developmental delays. An accurate device consistently adheres to the manufacturer-specified ratio.
- Volumetric Measurement of Water
Precise volumetric measurement of water is fundamental to achieving the correct formula concentration. Inaccurate water dispensing, even by small margins, can cumulatively affect the overall nutritional composition. For example, a device that consistently dispenses slightly less water than indicated can lead to a gradual over-concentration of the formula over multiple feedings.
- Powder Dispensing Mechanisms
The method by which the device dispenses formula powder significantly influences accuracy. Some devices utilize volumetric scoops, while others employ weight-based systems. Inherent variations in powder density can introduce inaccuracies with volumetric systems. Weight-based systems, if properly calibrated and maintained, generally offer greater accuracy by measuring mass directly.
- Calibration and Maintenance
Consistent accuracy requires regular calibration and maintenance of the device. Over time, components may drift out of calibration, leading to inaccuracies in dispensing. Manufacturers typically provide guidelines for calibration procedures. Adhering to these guidelines ensures the device continues to deliver the intended formula concentration.
The aspects discussed represent a critical chain that guarantees the accuracy of an automated infant formula preparation device. Failure at any stage of the process compromises the nutritional balance and compromises the device’s suitability for the task. Devices that excel in these measures contribute to nutritional consistency and reduce the risk of errors in formula preparation.
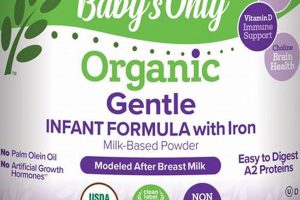
3. Compatibility
Compatibility, in the context of automated infant formula preparation devices, signifies the appliance’s ability to function correctly and safely with a range of formula types. This factor is essential in determining the suitability of a given device, as not all formulas are created equal and can vary substantially in their composition and physical properties. The lack of compatibility can lead to operational failures, inconsistent mixture preparation, or even damage to the appliance itself. For instance, a device designed for powdered formulas may be incompatible with concentrated liquid formulas, leading to clogging or inaccurate dispensing. A thorough understanding of a device’s compatibility is, therefore, critical for its effective and safe utilization.
The ramifications of incompatibility extend beyond mere operational inconveniences. The use of an incompatible formula may result in inaccurate nutrient concentrations, potentially leading to underfeeding or overfeeding, with corresponding negative impacts on infant growth and development. For example, a device not designed to handle formulas with a high concentration of certain thickeners may consistently dispense an incorrect ratio of formula to water. Furthermore, the physical characteristics of some formulas, such as their propensity to clump or foam, can interact negatively with certain dispensing mechanisms, causing further inconsistencies in preparation. Consequently, consideration of formula compatibility is not simply a matter of operational efficiency but rather a crucial aspect of ensuring proper infant nutrition.
The selection of an automated formula preparation device must, therefore, begin with a comprehensive assessment of its compatibility with the intended formula. Manufacturers typically provide lists of compatible formula types, and these should be carefully reviewed. Moreover, observing the device’s performance with the selected formula during initial use is advisable, paying particular attention to the consistency of the mixture and the absence of operational issues. Ultimately, the “best baby formula maker” is defined, in part, by its flexibility and reliability in handling diverse formula types without compromising safety or nutritional accuracy. This ensures that the device remains a useful tool for infant feeding regardless of changes in formula selection.
4. Consistency
Consistency is a critical attribute of any automated infant formula preparation device, as it directly impacts the nutritional well-being of the infant. A device demonstrating reliable and uniform preparation minimizes variability in nutrient concentrations, thereby contributing to stable growth and development. The “best baby formula maker” should, by definition, consistently produce formula bottles with the same composition, volume, and temperature across multiple preparations. This eliminates the potential for over- or under-concentration, which can lead to digestive issues, electrolyte imbalances, or inadequate caloric intake. Consistent formula preparation offers a predictable feeding experience, reducing the risk of discomfort or adverse reactions in sensitive infants.
One practical application of consistent preparation is evident in managing infants with specific dietary needs or sensitivities. For example, an infant with a cow’s milk protein allergy relies on precisely prepared hypoallergenic formula to avoid adverse reactions. A device that consistently delivers the correct concentration of this specialized formula is essential for maintaining the infant’s health. Furthermore, consistent temperature control prevents scalding and ensures the formula is palatable, encouraging the infant to consume the entire bottle. Variability in temperature can affect protein structure and nutrient availability, impacting the digestibility and nutritional value of the prepared formula. Therefore, consistent performance is not merely a matter of convenience but a core requirement for safe and effective infant feeding.
Achieving true consistency presents challenges for manufacturers of automated formula preparation devices. Factors such as variations in powder density, humidity, and water temperature can influence the dispensing accuracy. Furthermore, the design and maintenance of the device’s internal mechanisms play a crucial role in ensuring consistent performance over time. Despite these challenges, the “best baby formula maker” must prioritize consistent delivery to provide parents and caregivers with confidence in the quality and safety of each prepared bottle. This requires rigorous testing, quality control, and clear communication regarding proper maintenance and usage guidelines.
5. Ease of use
Ease of use is a critical attribute influencing the value and market acceptance of automated infant formula preparation devices. The “best baby formula maker” is characterized by intuitive operation, streamlined setup, and minimal maintenance requirements. Complex interfaces, lengthy cleaning procedures, or difficult assembly diminish user satisfaction and reduce the likelihood of consistent, correct usage. Devices that require extensive training or possess convoluted controls are less likely to be embraced by caregivers, particularly those experiencing sleep deprivation or time constraints. The simpler the operation, the greater the likelihood of consistent and accurate formula preparation.
Consider the scenario of a new parent needing to prepare a bottle in the middle of the night. A device requiring multiple steps, precise measurements, or specialized knowledge introduces opportunities for error and frustration. Conversely, a “best baby formula maker” features simplified operation, such as one-button activation, pre-programmed settings, and automatic cleaning cycles. These features minimize the cognitive load on the user, enabling rapid and accurate formula preparation even under challenging circumstances. Ease of use also extends to cleaning and maintenance. Devices with easily disassembled and dishwasher-safe components encourage regular cleaning, promoting hygiene and extending the device’s lifespan. Complexity in cleaning leads to infrequent maintenance, increasing the risk of bacterial contamination and mechanical failure.
In summation, ease of use is inextricably linked to the effectiveness and overall value of automated infant formula preparation devices. The “best baby formula maker” prioritizes intuitive design, simplified operation, and minimal maintenance to ensure consistent, accurate, and safe formula preparation. Devices lacking in these areas face reduced user adoption and may compromise the nutritional well-being of the infant. Therefore, manufacturers must prioritize user-centric design principles to create devices that are both technologically advanced and effortlessly simple to operate.
6. Safety
The association between safety and an automated infant formula preparation device, implicitly identified as the “best baby formula maker,” is foundational. Safety considerations encompass multiple aspects, including material composition, operational safeguards, and thermal management. Failure to address any of these areas introduces potential hazards. For instance, components constructed from materials that leach harmful chemicals into the formula present a direct threat to infant health. Similarly, inadequate thermal controls can result in scalding, leading to severe burns. A design lacking operational safeguards, such as automatic shutoff mechanisms, increases the risk of malfunctions that could compromise the formula’s integrity or cause injury.
Effective safety engineering mitigates these risks through rigorous testing and adherence to established safety standards. The use of BPA-free and phthalate-free materials minimizes the potential for chemical contamination. Precise temperature regulation, coupled with automatic shutoff features, prevents overheating and ensures the formula is prepared at a safe temperature for consumption. Robust construction and stable design reduce the likelihood of tipping or accidental spills, further enhancing safety. These features contribute to the reliability and security of the device, fostering caregiver confidence and promoting safe infant feeding practices. A device prioritizing these considerations reduces the potential for adverse events associated with formula preparation, thereby promoting infant well-being. Devices that neglect these considerations are inherently unsafe.
In conclusion, safety is not merely an ancillary feature but an intrinsic component of the “best baby formula maker.” It necessitates a comprehensive approach encompassing material selection, operational design, and adherence to stringent safety protocols. The consequences of neglecting safety range from minor discomfort to severe injury, underscoring the critical importance of prioritizing this aspect in the design, manufacturing, and utilization of these devices. A lack of stringent safety measures compromises the formula’s integrity and exposes the infant to potential harm.
7. Durability
Durability, referring to the prolonged functionality and resistance to degradation of the device over time, constitutes a significant factor in evaluating automated infant formula preparation systems. The longevity and consistent performance of such a device directly impact its overall value and utility to the consumer. Therefore, an understanding of the elements contributing to the durability of these systems is paramount.
- Material Composition and Resistance to Degradation
The materials utilized in the construction of an automated formula preparation device directly influence its lifespan. High-quality plastics, stainless steel, and other durable materials are resistant to cracking, warping, and chemical degradation from repeated exposure to water, formula, and cleaning agents. Inferior materials may break down over time, leading to leaks, inaccurate measurements, or complete system failure. For example, a device with a water tank constructed from brittle plastic is prone to cracking, rendering the system unusable.
- Mechanical Component Reliability
Automated formula preparation devices contain moving parts, such as pumps, mixers, and dispensing mechanisms. The reliability of these components under sustained use is crucial for maintaining consistent performance. High-quality motors, robust gears, and properly sealed components minimize the risk of failure due to wear and tear. A device with a poorly designed pump, for instance, may experience reduced dispensing accuracy or complete pump failure over time.
- Resistance to Wear from Cleaning and Maintenance
The cleaning and maintenance requirements of an automated formula preparation device can impact its durability. Components designed for easy disassembly and cleaning, using materials resistant to harsh cleaning agents, are less likely to degrade over time. A device with intricate crevices that are difficult to clean may accumulate residue, leading to bacterial growth and eventual component failure. Similarly, components susceptible to damage from common cleaning agents will require more frequent replacement, reducing the device’s overall lifespan.
- Design for Longevity and Repairability
The overall design of the device can contribute to its durability and ease of repair. Modular designs, with easily replaceable components, extend the lifespan of the system by allowing for targeted repairs. A device with a sealed, non-serviceable design may require complete replacement in the event of a single component failure. Furthermore, a design that protects sensitive components from moisture and physical damage enhances the device’s overall resilience.
The facets represent interconnected elements of a durable automated infant formula preparation device. The quality of materials, the robustness of mechanical components, the design for ease of cleaning and maintenance, and the overall design for longevity all contribute to the system’s ability to function reliably over an extended period. A system that excels in these areas provides a greater return on investment and offers a more sustainable solution for infant feeding.
Frequently Asked Questions
The following addresses common queries and concerns regarding automated infant formula preparation devices. The information is intended to provide clarity and promote informed decision-making regarding their use.
Question 1: What are the primary advantages of utilizing an automated infant formula preparation device?
Automated devices offer the potential for improved accuracy in formula-to-water ratios, reduced preparation time, and increased consistency compared to manual methods. These benefits can contribute to standardized feeding practices.
Question 2: What potential risks are associated with automated formula preparation devices?
Risks include bacterial contamination due to inadequate cleaning, inaccurate dispensing leading to nutritional imbalances, and potential exposure to harmful chemicals if the device is constructed from substandard materials.
Question 3: How frequently should an automated formula preparation device be cleaned?
Cleaning frequency should adhere strictly to the manufacturer’s recommendations. Daily cleaning of key components is generally advised, with more thorough disinfection performed on a weekly basis.
Question 4: Is it necessary to use distilled or purified water in automated formula preparation devices?
The utilization of distilled or purified water is highly recommended to minimize the risk of introducing contaminants that may be present in tap water. Consult the device’s manual for specific water quality recommendations.
Question 5: How can one ensure the accuracy of an automated formula preparation device?
Regular calibration, adherence to recommended formula-to-water ratios, and verification of dispensed volume are essential. Discrepancies should be addressed immediately, potentially requiring recalibration or repair.
Question 6: Are all infant formula types compatible with automated preparation devices?
No. Compatibility varies depending on the device. Consult the device’s documentation and the formula manufacturer to verify compatibility before use. Using an incompatible formula can lead to operational problems and inaccurate dispensing.
In summary, while automated infant formula preparation devices offer potential benefits, vigilant attention to hygiene, accuracy, and compatibility is crucial to ensure safe and effective utilization.
The subsequent discourse will consider the future trends in automated formula preparation technology.
Conclusion
This discussion has explored various facets of automated infant formula preparation devices, often referenced as the “best baby formula maker.” Critical aspects such as hygiene, accuracy, compatibility, ease of use, safety, and durability have been examined, emphasizing their influence on the device’s efficacy and potential benefits to infant feeding. Understanding these elements enables informed decision-making regarding the selection and utilization of such appliances.
The ongoing evolution of technology and infant nutritional science suggests continuous advancements in this domain. Vigilant monitoring of emerging research, adherence to established safety standards, and a commitment to informed practices remain paramount. The goal is to harness technological innovation responsibly, ensuring the well-being and optimal development of infants through safe and consistent feeding practices. The future demands a discerning approach, prioritizing evidence-based practices and robust safety measures in the application of these devices.