The selection of infant nutrition tailored for delicate digestive systems represents a crucial decision for caregivers. These specialized formulas are designed to alleviate discomfort often associated with sensitivities to common ingredients found in standard infant formulas, such as lactose or certain proteins. These formulas often incorporate hydrolyzed proteins, which are broken down into smaller, more easily digestible pieces, reducing the likelihood of allergic reactions or digestive distress. Examples include formulas with partially or extensively hydrolyzed whey or casein proteins.
Addressing dietary sensitivities in infancy is paramount for promoting optimal growth and development. Colic, gas, and excessive crying are potential indicators of underlying sensitivities, and appropriate formula selection can significantly improve infant well-being and parental peace of mind. Historically, advancements in food science have led to the development of increasingly sophisticated formulas that cater to a wider range of infant needs, reflecting an evolving understanding of infant physiology and nutritional requirements. This has resulted in a landscape of specialized products aimed at supporting infants with specific digestive challenges.
Therefore, a detailed examination of the options available becomes essential. The following sections will delve into key considerations when choosing an appropriate formula, explore common ingredients and their impact, and offer guidance on navigating the complexities of the infant formula market to best meet the needs of a sensitive infant.
Guidance on Selecting Suitable Infant Nutrition for Sensitivities
This section provides several key considerations for those navigating the landscape of infant formulas designed for sensitive digestive systems. Careful assessment of ingredients and individual infant needs is paramount.
Tip 1: Consult a Pediatrician. Prior to making any changes to an infant’s diet, seek professional medical advice. A pediatrician can assess the infant’s symptoms, diagnose potential sensitivities, and recommend appropriate formula options based on individual needs and medical history.
Tip 2: Understand Hydrolyzed Proteins. These proteins are broken down into smaller pieces, making them easier to digest and less likely to trigger allergic reactions. Extensively hydrolyzed formulas are typically recommended for infants with diagnosed cow’s milk protein allergy.
Tip 3: Consider Lactose Content. Lactose intolerance can contribute to digestive discomfort. Explore lactose-reduced or lactose-free formulas if lactose sensitivity is suspected. Monitor the infant for improved symptoms following the switch.
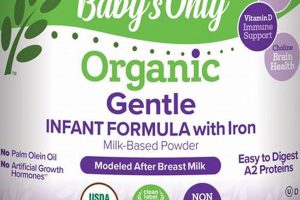
Tip 4: Evaluate Ingredient Lists. Scrutinize ingredient lists for potential allergens or irritants. Common culprits include soy, corn syrup solids, and artificial additives. Choose formulas with minimal ingredients and those that align with known sensitivities.
Tip 5: Monitor Infant Response. Introduce new formulas gradually and closely observe the infant for any adverse reactions, such as increased gas, diarrhea, skin rashes, or fussiness. Keep a detailed log of feeding times, amounts, and observed symptoms to facilitate accurate tracking.
Tip 6: Explore Different Brands. Different manufacturers utilize varying processes and ingredient combinations. If one product proves unsuitable, consider exploring alternative brands to find a formula that better aligns with the infant’s specific needs.
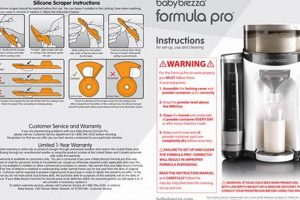
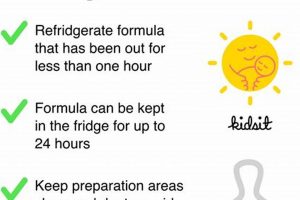
Tip 7: Prepare Formula Correctly. Always follow the manufacturer’s instructions precisely when preparing formula. Improper mixing or storage can compromise the formula’s nutritional value and potentially contribute to digestive upset. Use sterile water and bottles, especially for newborns.
Selecting appropriate nutrition for sensitive infants requires diligent research, professional guidance, and careful monitoring. By adhering to these tips, caregivers can make informed decisions that promote optimal infant health and well-being.
The following sections will further elaborate on specific formula types and address common concerns associated with sensitive digestive systems in infants.
1. Hydrolyzed Protein
Hydrolyzed protein is a crucial component of many formulas marketed as the “best sensitive baby formula” due to its altered protein structure. The process of hydrolysis breaks down the complex protein molecules into smaller peptides and amino acids. This modification reduces the allergenic potential of the protein, primarily cow’s milk protein, making it easier for infants with sensitivities or allergies to digest. The cause is the infant’s immature or compromised digestive system being unable to effectively break down intact proteins, leading to symptoms like colic, gas, diarrhea, and skin rashes. The effect is a reduction in these symptoms when a hydrolyzed protein formula is used.
The importance of hydrolyzed protein stems from its direct impact on reducing the immune system’s response to dietary proteins. In a standard formula, the infant’s immune system may recognize intact cow’s milk proteins as foreign substances, triggering an allergic reaction. By using hydrolyzed protein, the immune system is less likely to react, allowing the infant to absorb the nutrients without adverse effects. For example, an infant diagnosed with cow’s milk protein allergy will likely require an extensively hydrolyzed formula where proteins are broken down to a greater extent compared to a partially hydrolyzed formula used for infants with milder sensitivities. Real-life examples include infants who experienced significant symptom improvement, such as reduced crying and improved sleep, after switching to a hydrolyzed protein formula.
In summary, the practical significance of understanding the connection between hydrolyzed protein and the selection of a “best sensitive baby formula” lies in its ability to alleviate digestive distress and promote healthy growth and development in infants with protein sensitivities. However, selecting the appropriate degree of hydrolysis (partially versus extensively) requires careful consideration and consultation with a pediatrician to ensure the infant’s specific needs are adequately met. While hydrolyzed protein is beneficial, it may not be the sole solution for all sensitivities, and other factors like lactose content and added prebiotics/probiotics should also be evaluated.
2. Lactose Reduction
Lactose reduction, or its complete removal, plays a significant role in specialized infant formulas designed for sensitivities. Lactose, a disaccharide present in milk, requires the enzyme lactase for digestion. Some infants experience difficulty producing sufficient lactase, leading to lactose intolerance. This deficiency can result in gastrointestinal distress, manifesting as gas, bloating, diarrhea, and general discomfort. Consequently, formulas with reduced lactose content are frequently considered among the ‘best sensitive baby formula’ options, offering a potential solution to alleviate these symptoms.
The cause-and-effect relationship between lactose and infant distress highlights the importance of lactose reduction in specialized formulas. Lactose intolerance, whether primary (genetic) or secondary (resulting from infection or intestinal damage), can significantly impact an infant’s well-being. Formulating products with lower lactose levels can mitigate these negative effects. For instance, infants experiencing persistent colic or frequent loose stools may benefit from a switch to a lactose-reduced formula. Success stories often involve improvements in feeding tolerance and a reduction in crying spells following the transition. The availability of lactose-free or lactose-reduced options empowers caregivers to proactively manage potential digestive issues in their infants, improving overall quality of life.
However, it is crucial to acknowledge that not all infant sensitivities are attributable to lactose. Other factors, such as protein sensitivities or intolerances to other components within standard formulas, can also contribute to digestive problems. Therefore, lactose reduction is often one element within a more comprehensive approach to managing sensitive digestive systems. Pediatricians should be consulted to determine the underlying cause of an infant’s symptoms and to guide the appropriate formula selection. While lactose-reduced formulas offer a valuable tool in addressing some sensitivities, a holistic assessment is paramount to ensure the chosen formula aligns with the infant’s specific needs, as the best sensitive baby formula is the one most appropriate for the child.
3. Added Probiotics
The inclusion of probiotics in infant formula, particularly within the category of “best sensitive baby formula,” stems from the understanding of the gut microbiome’s critical role in infant health. Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. The rationale behind their addition is to positively influence the infant’s developing gut microbiota, potentially mitigating digestive discomfort and bolstering immune function. The underlying cause is often an immature or unbalanced gut microbiome in infants, which can lead to symptoms such as gas, colic, and diarrhea. The intended effect is to introduce beneficial bacteria that can colonize the gut, compete with harmful bacteria, and promote a more balanced microbial environment. For example, certain strains of Bifidobacterium and Lactobacillus are commonly added to infant formulas due to their demonstrated ability to reduce the incidence of gastrointestinal issues and support immune system development.
The importance of probiotics as a component of “best sensitive baby formula” lies in their potential to alleviate common digestive symptoms associated with formula feeding. Studies have shown that specific probiotic strains can reduce the duration of infantile colic and decrease the frequency of regurgitation. Moreover, probiotics can enhance the infant’s immune response by stimulating the production of antibodies and modulating the activity of immune cells. In real-life scenarios, infants fed with probiotic-supplemented formulas often exhibit fewer instances of antibiotic use, suggesting a strengthened immune system. However, it’s vital to note that not all probiotics are created equal. The efficacy of a probiotic depends on the specific strain, the dosage, and the infant’s individual gut microbiome composition. Therefore, selecting a formula with well-researched probiotic strains is crucial for maximizing potential benefits. Practical application also involves careful monitoring of the infant’s response to the formula and consulting with a pediatrician to determine the most appropriate probiotic strain and dosage.
In summary, the incorporation of added probiotics into “best sensitive baby formula” is a targeted approach to address imbalances in the infant gut microbiome, potentially reducing digestive discomfort and enhancing immune function. The selection of a formula with probiotics should be based on scientific evidence supporting the efficacy of specific strains. While probiotics offer a promising avenue for improving infant health, they are not a universal solution, and their effectiveness can vary depending on individual factors. Challenges include determining the optimal probiotic strain and dosage for each infant and ensuring the viability of probiotics during formula production and storage. Nonetheless, added probiotics remain a valuable consideration when selecting infant nutrition designed to support sensitive digestive systems, in conjunction with other factors like hydrolyzed protein and reduced lactose content. Consultation with a pediatrician remains paramount.
4. Reduced Allergen
The concept of “reduced allergen” is intrinsically linked to the selection of “best sensitive baby formula”. The presence of allergens in standard infant formulas can trigger adverse reactions in susceptible infants, manifesting as gastrointestinal distress, skin rashes, or respiratory symptoms. Formulas designed with reduced allergen content aim to minimize the risk of these reactions by excluding or modifying common allergenic ingredients. The underlying cause is the infant’s immune system reacting to specific proteins, most frequently those found in cow’s milk or soy. The effect of utilizing a reduced allergen formula is a decreased likelihood of triggering an allergic response, resulting in improved tolerance and well-being for the infant. For instance, extensively hydrolyzed formulas, where cow’s milk proteins are broken down into smaller, less allergenic fragments, are frequently recommended for infants with diagnosed cow’s milk protein allergy.
The importance of reduced allergen formulas lies in their ability to provide adequate nutrition while minimizing the risk of allergic reactions in sensitive infants. Clinical examples include cases where infants with recurrent eczema or persistent colic symptoms experienced significant improvement after transitioning to a reduced allergen formula, specifically one with hydrolyzed protein or free of cow’s milk and soy. Practically, this understanding empowers caregivers and healthcare professionals to make informed decisions regarding formula selection, tailoring the choice to the individual infant’s needs and sensitivities. This proactive approach can prevent unnecessary discomfort and promote optimal growth and development. Formula manufacturers may employ various strategies to reduce allergen content, including protein hydrolysis, amino acid-based formulations, and the exclusion of common allergens like soy, wheat, and nuts.
In summary, the emphasis on “reduced allergen” is a critical aspect of “best sensitive baby formula” selection. The goal is to provide a nutritionally complete product that minimizes the potential for allergic reactions in vulnerable infants. While reduced allergen formulas offer a valuable tool in managing sensitivities, accurate diagnosis of the specific allergen and consultation with a pediatrician are essential to ensure the chosen formula is appropriate for the individual infant’s needs. Challenges include identifying less common allergens and ensuring the complete removal of allergenic proteins during processing. Nonetheless, the focus on allergen reduction remains a cornerstone in the development and selection of formulas designed for infants with sensitivities, aligning with the broader aim of promoting infant health and well-being.
5. Doctor Recommended
The designation “Doctor Recommended” in the context of “best sensitive baby formula” signifies a crucial endorsement by medical professionals. This endorsement arises from a pediatrician’s or other qualified healthcare provider’s assessment of the formula’s suitability for infants with specific digestive sensitivities or allergies. The cause of this recommendation typically stems from the formula’s composition, which may include hydrolyzed proteins, reduced lactose, or the absence of common allergens. The intended effect is to alleviate the infant’s symptoms, improve their tolerance of the formula, and promote healthy growth and development. A doctor’s recommendation is often based on clinical experience, published research, and guidelines from pediatric associations, lending a degree of credibility to the formula’s effectiveness and safety.
The importance of the “Doctor Recommended” aspect lies in the potential for a tailored and informed approach to infant nutrition. While marketing claims may influence consumer choices, a doctor’s recommendation is predicated on a professional evaluation of the infant’s individual needs and medical history. Real-life examples include infants who have experienced a marked improvement in symptoms, such as reduced colic or resolution of allergic skin reactions, after switching to a formula specifically recommended by their pediatrician. The practical significance of this understanding is that it encourages parents and caregivers to seek professional medical advice before making significant dietary changes for their infant, thereby minimizing the risk of adverse reactions and optimizing nutritional outcomes. Furthermore, “Doctor Recommended” can provide assurance to parents overwhelmed by the numerous formula options available, offering a validated starting point in their selection process.
In conclusion, the association between “Doctor Recommended” and “best sensitive baby formula” underscores the value of expert medical guidance in navigating the complexities of infant nutrition. While a doctor’s recommendation does not guarantee success for every infant, it represents a conscientious and evidence-based approach to addressing digestive sensitivities and allergies. Challenges exist in ensuring consistent and unbiased recommendations across different healthcare providers, as well as in keeping abreast of the latest research and product innovations. Nonetheless, the emphasis on “Doctor Recommended” reinforces the broader theme of prioritizing infant health and well-being through informed decision-making and personalized care, making it a critical consideration in the search for the ideal formula.
6. Infant Tolerance
Infant tolerance serves as the ultimate litmus test for any formula claiming to be the “best sensitive baby formula.” Despite meticulously crafted ingredient lists and doctor recommendations, the infant’s physiological response dictates the true suitability of a given product. Evaluating tolerance involves careful observation and documentation of various physical and behavioral indicators.
- Gastrointestinal Response
Gastrointestinal response represents a primary indicator of infant tolerance. Frequent regurgitation, excessive gas, constipation, or diarrhea suggest potential intolerance. For example, an infant experiencing persistent diarrhea after initiating a new formula may exhibit an intolerance to a specific ingredient, necessitating a switch to an alternative option. Monitoring stool consistency and frequency provides valuable insight into digestive health. Formulations marketed as “best sensitive baby formula” must demonstrate a capacity to minimize these adverse gastrointestinal effects.
- Skin Manifestations
Skin manifestations can also signal formula intolerance. Eczema, hives, or other rashes developing after formula introduction may indicate an allergic reaction or sensitivity to an ingredient. For instance, an infant exhibiting a red, itchy rash around the mouth or on the body after consuming a particular formula may be reacting to cow’s milk protein or soy. Reduced allergen formulas are designed to mitigate these skin-related reactions, but vigilant observation remains crucial. The absence of adverse skin reactions is a key determinant of a well-tolerated “best sensitive baby formula”.
- Behavioral Cues
Behavioral cues offer another layer of assessment. Excessive crying, irritability, and sleep disturbances can reflect underlying discomfort associated with formula intolerance. For instance, an infant who consistently cries inconsolably after feedings, despite attempts at soothing, may be experiencing abdominal pain or discomfort due to a poorly tolerated formula. While crying can have multiple causes, a temporal relationship between feeding and increased fussiness warrants investigation. Formulas that promote calmness and restful sleep contribute significantly to the perception of being the “best sensitive baby formula”.
- Growth and Development
Adequate growth and development serve as long-term indicators of formula tolerance. A formula that supports healthy weight gain, length increase, and overall development is deemed well-tolerated. Conversely, failure to thrive or stunted growth may signal an underlying intolerance or inadequate nutrient absorption. Regular monitoring of growth parameters by a healthcare professional is essential to ensure the chosen formula adequately meets the infant’s nutritional needs. A “best sensitive baby formula” must demonstrably support optimal growth trajectories while minimizing adverse reactions.
Ultimately, “Infant Tolerance” is a multifaceted concept encompassing physiological and behavioral responses to a particular formula. The absence of gastrointestinal distress, skin manifestations, behavioral disturbances, and the presence of healthy growth patterns collectively contribute to a judgment of good tolerance. While labels and recommendations can guide initial choices, direct observation of the infant’s response remains paramount in determining whether a given formula truly qualifies as the “best sensitive baby formula” for that individual. The absence of adverse effects, coupled with demonstrable growth and developmental progress, provides the most compelling evidence of formula suitability.
7. Nutritional Completeness
Nutritional completeness represents a non-negotiable requirement for any infant formula, including those marketed as the “best sensitive baby formula”. This concept encompasses the presence of all essential nutrients macronutrients (proteins, carbohydrates, and fats) and micronutrients (vitamins and minerals) in appropriate quantities to support optimal growth, development, and physiological function. The cause of this stringent requirement stems from the infant’s exclusive reliance on formula as the primary, and often sole, source of nutrition during the first months of life. The effect of providing a nutritionally complete formula is to ensure that the infant receives all the necessary building blocks for healthy development, preventing deficiencies and supporting robust immune function. An example illustrating this point involves infants exclusively fed a nutritionally inadequate formula, who may exhibit failure to thrive, developmental delays, and increased susceptibility to infections. These outcomes highlight the critical importance of nutritional completeness in infant formula selection.
Formulas marketed as “best sensitive baby formula” often undergo modifications to address specific digestive sensitivities, such as hydrolyzed proteins or reduced lactose content. However, these modifications must never compromise the formula’s overall nutritional profile. Manufacturers must ensure that any alterations retain or supplement the necessary nutrients to meet established guidelines set forth by regulatory bodies and pediatric organizations. For example, if lactose is reduced, the carbohydrate content must be adjusted with alternative sources to provide adequate energy for the infant. Another practical consideration involves ensuring that the processing methods used to create sensitive formulas do not inadvertently deplete essential vitamins or minerals. Regular testing and quality control are essential to guarantee that the final product meets stringent nutritional standards. Clinical research and rigorous formulation practices ensure the delivery of balanced nutrition even in specialized formulas.
In summary, the nexus between “Nutritional Completeness” and “best sensitive baby formula” is inextricably linked. Addressing digestive sensitivities must not come at the expense of providing all essential nutrients in appropriate quantities. Maintaining nutritional integrity is paramount to promoting optimal infant health and development. Challenges lie in formulating sensitive formulas that meet both digestive needs and nutritional requirements, necessitating careful ingredient selection, processing techniques, and quality control measures. The ongoing commitment to nutritional completeness ensures that infants receive the necessary building blocks for healthy growth and development, regardless of their specific dietary needs or sensitivities, reinforcing the objective of providing a “best sensitive baby formula” that truly supports overall well-being.
Frequently Asked Questions
This section addresses common inquiries regarding infant formula sensitivities, providing evidence-based information for informed decision-making.
Question 1: What defines “best sensitive baby formula,” and how does it differ from standard formulas?
Sensitive formulas are specifically designed to alleviate digestive discomfort in infants with sensitivities or allergies. These formulas often contain hydrolyzed proteins, reduced lactose, or are free from common allergens like soy. Standard formulas, while nutritionally complete, may contain intact proteins and higher lactose levels, potentially triggering adverse reactions in sensitive infants.
Question 2: How can one determine if an infant requires “best sensitive baby formula”?
Signs indicating a potential need for sensitive formula include persistent colic, excessive gas, diarrhea, constipation, eczema, or a family history of allergies. However, a definitive diagnosis and recommendation should be made by a pediatrician based on a thorough evaluation of the infant’s symptoms and medical history. Self-diagnosis is not recommended.
Question 3: Are all “best sensitive baby formula” options lactose-free?
No, not all sensitive formulas are lactose-free. Some formulas are lactose-reduced, while others utilize hydrolyzed proteins or alternative carbohydrate sources. The specific type of sensitive formula required depends on the nature of the infant’s sensitivity. Lactose intolerance is only one potential cause of digestive distress.
Question 4: Can “best sensitive baby formula” completely eliminate allergic reactions?
While sensitive formulas, particularly extensively hydrolyzed or amino acid-based formulas, significantly reduce the risk of allergic reactions, they cannot guarantee complete elimination. Some infants may still exhibit sensitivities to other ingredients or trace amounts of allergens. Close monitoring and consultation with a pediatrician are crucial.
Question 5: Are “best sensitive baby formula” options nutritionally equivalent to standard formulas?
Reputable sensitive formulas are designed to be nutritionally complete, providing all the essential nutrients required for infant growth and development. However, it is imperative to verify that the chosen formula meets established nutritional guidelines and to monitor the infant’s growth parameters to ensure adequate nutrition.
Question 6: Should a “best sensitive baby formula” be chosen based solely on marketing claims?
Relying solely on marketing claims is strongly discouraged. Selecting an appropriate formula requires careful consideration of the infant’s individual needs, a thorough review of the ingredient list, and, most importantly, guidance from a qualified healthcare professional. Marketing claims should be viewed as supplementary information, not the primary basis for decision-making.
In summary, the selection of infant formula tailored for sensitive digestive systems necessitates a data-driven methodology, prioritizing the well-being of the child.
The subsequent section offers more detailed information on each formula element.
Best Sensitive Baby Formula
The preceding exploration of “best sensitive baby formula” has underscored the complexity inherent in selecting appropriate infant nutrition for delicate digestive systems. Key considerations encompass hydrolyzed protein content, lactose reduction strategies, probiotic supplementation, allergen minimization, medical professional recommendations, infant tolerance, and nutritional completeness. A balanced approach, accounting for each of these elements, is paramount.
Ultimately, the selection of the most suitable formula remains a critical decision, impacting infant health and well-being. Caregivers are urged to consult with pediatricians or other qualified healthcare providers to obtain personalized guidance. Continued research and advancements in infant nutrition will undoubtedly lead to further refinements in specialized formulas, offering improved options for infants with sensitivities and allergies. Prioritizing evidence-based decision-making and diligent monitoring of infant response will remain essential in optimizing nutritional outcomes.