The condition where a primary tooth exhibits mobility within the socket yet remains connected to the gum tissue is a common occurrence in childhood. This typically signifies the natural process of exfoliation, wherein the permanent tooth underneath is resorbing the root of the primary tooth. As an example, a child might wiggle a tooth that moves back and forth but doesn’t easily come out, indicating it is loose but still attached.
Understanding this stage of dental development is crucial for both parents and children. It highlights the body’s inherent mechanisms for preparing the mouth for permanent dentition. Historically, this stage was often met with anxiety, but with modern dental education, it’s now generally viewed as a normal and expected part of growing up. Facilitating proper oral hygiene during this time minimizes the risk of infection and discomfort.
Subsequent sections will address recommended practices for managing this transitional phase, potential complications that might arise, and when professional dental intervention is necessary. The objective is to provide guidance on ensuring a smooth and healthy transition from primary to permanent teeth.
Managing a Mobile Primary Tooth
This section provides guidance on managing a situation where a primary tooth is loose but still attached. The advice aims to ensure comfort, prevent complications, and promote healthy oral hygiene during this natural process.
Tip 1: Encourage Gentle Wiggling. Encourage the child to gently wiggle the loose tooth with their tongue or a clean finger. This can help accelerate the natural loosening process. However, avoid forceful pulling, which could cause unnecessary pain or bleeding.
Tip 2: Maintain Excellent Oral Hygiene. Continue brushing and flossing as usual. Pay particular attention to the area around the loose tooth to remove food particles and plaque. A soft-bristled toothbrush is recommended to minimize irritation.
Tip 3: Offer Soft Foods. During meals, offer soft foods that require minimal chewing. This reduces pressure on the loose tooth and minimizes discomfort. Examples include mashed potatoes, yogurt, and cooked vegetables.
Tip 4: Rinse with Warm Salt Water. After meals, have the child rinse their mouth with warm salt water (approximately 1/4 teaspoon of salt in a cup of warm water). This helps to soothe the gums and prevent infection.
Tip 5: Avoid Sticky or Chewy Candies. Discourage the consumption of sticky or chewy candies, as these can pull on the loose tooth and cause pain or premature detachment.
Tip 6: Monitor for Excessive Bleeding. A small amount of bleeding is normal if the tooth comes out. However, if there is excessive bleeding that does not stop after applying gentle pressure with a clean gauze pad for 15-20 minutes, consult a dentist.
Tip 7: Consult a Dentist if Necessary. If the tooth is causing significant pain, is interfering with eating or speaking, or shows signs of infection (redness, swelling, pus), schedule an appointment with a dentist. Professional evaluation is crucial in these situations.
Adhering to these tips will help facilitate a comfortable and healthy transition as the primary tooth completes its natural exfoliation process. Maintaining proper oral hygiene and observing for potential complications are essential for optimal dental health.
The following sections will delve into possible complications, preventive measures, and when to seek professional dental consultation.
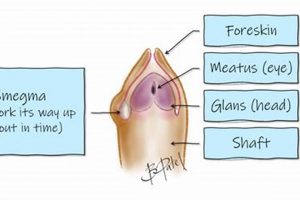
1. Mobility assessment
Mobility assessment, in the context of a primary tooth that is loose but still attached, serves as a critical diagnostic step in determining the stage of exfoliation and potential need for intervention. The degree of movement provides valuable information regarding the extent of root resorption by the underlying permanent tooth. A tooth exhibiting slight mobility may indicate early stages of the natural shedding process, whereas significant mobility, where the tooth is barely attached, can signify advanced resorption. Understanding the correlation between mobility and attachment provides an objective measure of the tooth’s stability and assists in distinguishing normal physiological processes from potentially problematic scenarios. For instance, if a primary tooth shows minimal mobility at an age when exfoliation is expected, it may warrant further investigation to rule out issues such as ankylosis or impaction of the permanent successor.
The practical application of mobility assessment extends to both clinical practice and home monitoring. Dental professionals utilize specialized instruments and techniques to quantify the extent of tooth movement. Parents can be educated to observe and track the mobility of their child’s loose tooth, noting any changes or abnormalities. This proactive approach allows for timely detection of potential complications, such as premature loss of the primary tooth due to trauma, which could necessitate space maintenance procedures to prevent malocclusion. Furthermore, understanding the range of normal mobility associated with exfoliating primary teeth helps alleviate parental anxiety and reduces the likelihood of unnecessary dental visits.
In summary, mobility assessment plays a pivotal role in the evaluation of a primary tooth that is loose but still attached. This assessment provides vital insights into the physiological status of the tooth, facilitates appropriate management strategies, and promotes informed decision-making regarding the need for professional dental care. A systematic approach to assessing mobility ensures that potential complications are identified and addressed promptly, contributing to the overall oral health and development of the child.
2. Attachment Strength
Attachment strength, in the context of a mobile primary tooth, denotes the degree to which the tooth remains connected to the surrounding gingival tissues and alveolar bone. This parameter is crucial in assessing the tooth’s readiness for exfoliation and guiding appropriate management strategies. Diminished attachment strength is characteristic of a tooth undergoing natural root resorption, but variations can indicate underlying dental issues.
- Role of Periodontal Ligament Fibers
The periodontal ligament, composed of collagen fibers, anchors the tooth to the alveolar bone. Attachment strength is directly correlated with the integrity of these fibers. As the permanent tooth erupts, it stimulates osteoclastic activity, leading to the breakdown of the primary tooth’s root and subsequent weakening of the periodontal ligament. For example, if a primary tooth exhibits minimal attachment due to extensive root resorption, it may be easily displaced with minimal force. Conversely, persistent attachment strength despite mobility could suggest ankylosis or fusion of the tooth to the bone.
- Influence of Root Resorption Patterns
The pattern of root resorption significantly impacts attachment strength. Uniform resorption, where the root is gradually dissolved, typically results in a predictable decrease in attachment. Irregular resorption, often observed in cases of ectopic eruption of the permanent successor or infection, can create areas of localized weakness, affecting attachment unevenly. Clinically, a tooth with irregular resorption might exhibit varying degrees of mobility and attachment along different surfaces.
- Impact of Inflammatory Processes
Inflammation, resulting from poor oral hygiene or localized infection, can compromise attachment strength. Inflammatory mediators degrade collagen fibers in the periodontal ligament, accelerating the loosening of the tooth. For instance, gingivitis around a loose primary tooth can exacerbate attachment loss, increasing the risk of premature exfoliation or pain. Managing inflammation through meticulous oral hygiene practices is essential for preserving the remaining attachment and preventing further complications.
- Significance of Cementum and Dentin Integrity
Cementum, the outer layer of the root, and dentin, the underlying tissue, contribute to the tooth’s overall structural integrity and attachment. Root resorption gradually diminishes these components, weakening the tooth’s anchorage. Pathological conditions, such as internal resorption or carious lesions, can further compromise cementum and dentin, leading to a rapid decline in attachment strength. In these cases, prompt dental intervention is necessary to address the underlying pathology and prevent further damage.
The facets of attachment strength collectively provide a comprehensive understanding of the dynamics involved when a primary tooth is loose but still attached. By considering the integrity of the periodontal ligament, root resorption patterns, inflammatory processes, and the condition of cementum and dentin, clinicians and caregivers can effectively assess the tooth’s status and implement appropriate strategies to promote a healthy transition to the permanent dentition. Monitoring these parameters is crucial for identifying potential complications and ensuring optimal oral health outcomes.
3. Discomfort Level
The discomfort level associated with a primary tooth that is loose but still attached represents a crucial indicator of the underlying physiological processes and potential complications. Pain or sensitivity often arises due to the gradual resorption of the tooth’s root structure and the subsequent inflammation of the surrounding gingival tissues. For example, a child might experience mild discomfort during chewing or when the loose tooth is inadvertently touched. The intensity of discomfort can vary based on factors such as the degree of mobility, the presence of infection, and individual pain tolerance. In cases where the loose tooth is impinging on adjacent tissues or interfering with normal oral function, the discomfort level may escalate, necessitating prompt dental evaluation.
Evaluating discomfort level is an essential component in managing a mobile primary tooth. Parents and caregivers should monitor the child’s subjective reports of pain, as well as observe for objective signs such as reluctance to eat, frequent touching of the tooth, or altered speech patterns. A thorough clinical examination by a dentist can help determine the source of discomfort and rule out underlying pathologies. For instance, if the discomfort is disproportionate to the tooth’s mobility, it could indicate the presence of a periapical infection or trauma. Conversely, minimal discomfort despite significant mobility might suggest adequate root resorption and impending exfoliation. Non-pharmacological interventions, such as soft food diets and warm saline rinses, can provide symptomatic relief. In severe cases, analgesics or professional removal of the tooth may be required.
In summary, the discomfort level associated with a primary tooth that is loose but still attached is a significant clinical parameter that reflects the dynamic interplay between physiological processes and potential pathological conditions. By carefully assessing and managing discomfort, clinicians and caregivers can ensure optimal comfort, prevent complications, and promote a smooth transition to the permanent dentition. While mild discomfort is often a normal part of the exfoliation process, escalating or persistent pain warrants prompt dental evaluation to address underlying issues and prevent long-term sequelae. The challenges associated with managing discomfort underscore the importance of proactive monitoring, meticulous oral hygiene, and timely professional intervention.
4. Oral Hygiene
Maintaining meticulous oral hygiene during the period when a primary tooth is loose but still attached is crucial for preventing complications and promoting a healthy transition to permanent dentition. The presence of a mobile tooth creates unique challenges in plaque control and infection prevention, necessitating specific adjustments to routine oral care practices.
- Plaque Accumulation and Gingival Inflammation
A loose primary tooth can create areas where plaque and food particles easily accumulate, leading to gingival inflammation. The altered anatomy around the mobile tooth makes these areas difficult to clean effectively with regular brushing. For example, if plaque is not adequately removed, gingivitis can develop, characterized by redness, swelling, and bleeding of the gums. This inflammation can exacerbate the loosening process and increase discomfort.
- Risk of Infection
The presence of a loose tooth creates a potential entry point for bacteria into the surrounding tissues. If the gums are traumatized or if there is a break in the mucosal barrier, bacteria can cause localized infections. In severe cases, this can lead to cellulitis or even systemic infections. Maintaining good oral hygiene minimizes the bacterial load and reduces the risk of such infections. For instance, consistent rinsing with warm salt water can help to keep the area clean and promote healing.
- Impact on Adjacent Teeth
Poor oral hygiene around a loose primary tooth can also affect the adjacent teeth. Plaque and bacteria can spread to the neighboring teeth, increasing the risk of caries or gingivitis. The accumulation of debris can also hinder the eruption of the underlying permanent tooth. Proper oral hygiene, including flossing around the adjacent teeth, is essential for protecting their health. A specific example would be ensuring the interdental spaces are free of food debris to prevent proximal caries.
- Promoting Natural Exfoliation
While good oral hygiene cannot directly accelerate the exfoliation process, it helps to create an environment conducive to natural shedding. By preventing inflammation and infection, the natural resorption of the tooth root by the underlying permanent tooth can proceed unimpeded. If infection is present, the inflammatory response can interfere with the normal exfoliation process. Maintaining a clean oral environment supports the body’s natural mechanisms.
In conclusion, meticulous oral hygiene practices are paramount when managing a primary tooth that is loose but still attached. By preventing plaque accumulation, minimizing the risk of infection, protecting adjacent teeth, and supporting the natural exfoliation process, comprehensive oral hygiene contributes significantly to a smooth and healthy transition from primary to permanent dentition. Failure to maintain adequate oral hygiene can lead to complications that may necessitate professional dental intervention, underscoring the importance of diligent home care.
5. Potential causes
The condition wherein a primary tooth exhibits mobility while remaining attached to the gingival tissue arises from a spectrum of potential causes, each impacting the natural exfoliation process. Understanding these causes is crucial for appropriate management and intervention. Physiological root resorption, driven by the erupting permanent successor, is the most common and expected cause. This process involves odontoclasts, specialized cells, breaking down the root structure of the primary tooth, gradually weakening its attachment. However, other factors can contribute to a prematurely mobile primary tooth. Trauma, such as a direct blow to the mouth, can damage the periodontal ligament and supporting structures, leading to loosening. In such cases, the mobility may not be associated with root resorption but rather with acute injury.
Furthermore, pathological conditions can also initiate the loosening of a primary tooth. Periapical infections, often stemming from untreated caries, can spread to the periodontal tissues, causing inflammation and bone loss, which weakens the tooth’s attachment. Ectopic eruption of the permanent successor, where it erupts in an abnormal position, can lead to uneven or accelerated resorption of the primary tooth’s root, resulting in premature mobility. Systemic conditions, though less common, can also impact tooth stability. For instance, certain metabolic disorders or genetic syndromes may affect bone density or periodontal health, indirectly contributing to the loosening of primary teeth. The identification of the underlying cause through clinical examination and radiographic assessment is paramount for devising an effective treatment plan. This may involve monitoring the natural exfoliation process, managing infections, addressing traumatic injuries, or referring to specialists for systemic conditions.
In summary, the causes behind a mobile but still attached primary tooth are diverse, ranging from the physiological process of root resorption to traumatic injuries and underlying pathological conditions. A thorough understanding of these potential causes is essential for accurate diagnosis and appropriate management. Failing to recognize the specific etiology can lead to delayed or inappropriate interventions, potentially affecting the health and alignment of the permanent dentition. Consequently, a comprehensive evaluation that considers the patient’s medical and dental history, clinical findings, and radiographic evidence is imperative for ensuring optimal oral health outcomes.
6. Dental Evaluation
A comprehensive dental evaluation is crucial when addressing a primary tooth that is loose but still attached. Such evaluation facilitates informed decision-making regarding appropriate management and intervention strategies, ensuring optimal oral health outcomes.
- Clinical Assessment of Mobility and Attachment
During a dental evaluation, the clinician meticulously assesses the degree of tooth mobility and the strength of its remaining attachment to the surrounding tissues. This involves gentle manipulation of the tooth to gauge its movement in all directions. The assessment provides objective data on the extent of root resorption and helps differentiate between physiological loosening and pathological conditions. For example, significant mobility with minimal attachment may indicate advanced root resorption and impending exfoliation, while limited mobility despite parental concerns could point towards ankylosis or impaction. This clinical assessment forms the foundation for subsequent diagnostic and treatment planning steps.
- Radiographic Examination for Underlying Pathology
Radiographic imaging, such as periapical radiographs or panoramic radiographs, is frequently employed to evaluate the underlying structures and rule out potential complications. Radiographs allow visualization of the root morphology, the position of the erupting permanent successor, and the presence of any periapical pathology. For instance, a radiograph might reveal the presence of a periapical infection associated with the loose primary tooth, which would necessitate antibiotic treatment or extraction. Similarly, it can confirm the presence of a supernumerary tooth or an odontoma hindering the normal eruption pattern. The radiographic examination supplements the clinical assessment, providing a comprehensive understanding of the factors contributing to the loose tooth.
- Evaluation of Occlusion and Space Management
The dental evaluation also includes an assessment of the child’s occlusion and the available space for the erupting permanent teeth. Premature loss of a primary tooth can lead to drifting of adjacent teeth, resulting in space loss and subsequent malocclusion. The evaluation determines whether space maintenance is necessary to prevent future orthodontic problems. For example, if a primary molar is prematurely lost due to advanced caries, a space maintainer may be indicated to preserve the arch length and ensure proper alignment of the permanent teeth. The evaluation of occlusion and space is vital for long-term dental health.
- Assessment of Soft Tissues and Infection Control
During the examination, the clinician also evaluates the surrounding soft tissues for signs of inflammation, infection, or trauma. The presence of gingivitis, swelling, or purulent discharge indicates a need for improved oral hygiene and possibly antibiotic therapy. Furthermore, the evaluation identifies any sharp edges or rough surfaces on the loose tooth that could cause trauma to the tongue or cheeks. Addressing these issues prevents discomfort and reduces the risk of secondary infections. For example, smoothing a sharp edge on a fractured primary tooth can alleviate irritation and promote healing of the adjacent tissues. The soft tissue assessment ensures that the immediate oral environment is conducive to comfort and healing.
These interconnected facets of a dental evaluation are indispensable when a primary tooth is loose but still attached. The synthesis of clinical findings, radiographic evidence, and assessment of occlusion and soft tissues allows for informed decisions regarding management. This comprehensive approach promotes optimal oral health, minimizes the risk of complications, and guides the smooth transition to the permanent dentition.
Frequently Asked Questions
This section addresses common inquiries regarding the condition of a primary tooth that is loose but still attached. The responses provide information based on established dental practices.
Question 1: Is it normal for a baby tooth to be loose but still somewhat attached?
Yes, this is a common occurrence as permanent teeth develop and begin to resorb the roots of the primary teeth. The attachment gradually weakens until the primary tooth naturally exfoliates.
Question 2: What should be done if a loose baby tooth is causing discomfort?
Encourage gentle rinsing with warm salt water. A diet of soft foods may also minimize irritation. If discomfort persists or intensifies, a dental examination is warranted.
Question 3: Should a loose baby tooth be pulled out at home?
Forceful extraction is discouraged. Gentle wiggling with clean fingers may be permitted. However, allowing the tooth to exfoliate naturally is generally preferred to avoid trauma.
Question 4: How can infection around a loose baby tooth be prevented?
Maintaining meticulous oral hygiene is essential. This includes brushing and flossing carefully around the loose tooth to remove plaque and food debris. Warm salt water rinses can also aid in preventing infection.
Question 5: When should a dentist be consulted about a loose baby tooth?
A dental professional should be consulted if the tooth is causing significant pain, interfering with eating or speaking, displaying signs of infection (redness, swelling, pus), or if the permanent tooth erupts before the primary tooth is lost.
Question 6: Can a loose baby tooth affect the alignment of permanent teeth?
Premature loss of a primary tooth due to trauma or disease can potentially impact the alignment of permanent teeth. A dental evaluation can determine if space maintenance is necessary to prevent future orthodontic problems.
In summary, a loose but still attached primary tooth is often a normal part of dental development. Monitoring the situation, maintaining oral hygiene, and seeking professional advice when necessary are key to a smooth transition to permanent teeth.
The subsequent section will address potential complications and preventive measures related to loose primary teeth.
Conclusion
The phenomenon of a primary tooth exhibiting mobility while remaining attached signifies a critical phase in dental development. This exploration has illuminated the multifaceted nature of this common occurrence, underscoring the importance of assessing mobility, attachment strength, discomfort level, and maintaining rigorous oral hygiene. Potential causes, ranging from natural root resorption to traumatic injuries and underlying pathologies, necessitate careful consideration. Dental evaluation plays a pivotal role in discerning the etiology and formulating appropriate management strategies. The FAQ section has addressed common parental concerns, offering practical guidance on home care and indications for professional consultation.
Successfully navigating the period when a “baby tooth is loose but still attached” requires diligent monitoring and informed decision-making. Addressing this condition thoughtfully ensures a healthy transition to the permanent dentition, minimizing the risk of complications and fostering optimal oral health outcomes for the developing child. Consistent application of the principles outlined herein supports the long-term integrity of the dentition and contributes to a foundation of lifelong oral well-being.