Swaddling, a technique used to wrap infants snugly in a blanket, aims to mimic the feeling of being held, promoting calmness and sleep. However, applying excessive pressure during this process is possible, potentially leading to adverse physical effects. Constriction of the infant’s chest or hips beyond a safe range illustrates this concern.
Proper swaddling technique is critical for infant safety and well-being. Historically, swaddling has been practiced across various cultures, though methods have evolved. The contemporary understanding of infant physiology emphasizes the importance of allowing freedom of movement for healthy hip development and unrestricted breathing, making a gentle, secure wrap more desirable than an overly tight one.
The following sections will delve into the potential risks associated with overly restrictive swaddling practices, discuss methods for appropriate swaddling, and provide guidance on recognizing signs of discomfort or potential harm in a swaddled infant.
Swaddling Safety
Optimal swaddling balances security and freedom. Ensuring the infant’s well-being requires vigilant attention to technique and observation.
Tip 1: Prioritize Hip Health: Employ a swaddling method that allows for natural hip flexion and abduction. The legs should be able to move freely, avoiding being held straight and pressed together.
Tip 2: Assess Chest Restriction: Ensure sufficient space for comfortable breathing. The swaddle should not restrict chest expansion during respiration. Observe the infant’s breathing pattern after swaddling.
Tip 3: Use Breathable Fabrics: Select lightweight, breathable materials like cotton muslin. Overheating poses a risk, particularly when coupled with excessive swaddling tightness.
Tip 4: Monitor for Signs of Discomfort: Observe the infant for indicators of distress such as rapid breathing, skin discoloration, or attempts to escape the swaddle. Adjust the swaddle if these signs are present.
Tip 5: Avoid Over-Swaddling: Swaddling is not necessary for all naps or throughout the night. As the infant develops the ability to roll over, discontinue swaddling to prevent potential hazards.
Tip 6: Consider Environmental Factors: Adjust the tightness of the swaddle based on room temperature and the infant’s clothing to prevent overheating.
Tip 7: Seek Professional Guidance: Consult with a pediatrician or certified swaddling instructor for personalized recommendations and technique validation.
Preventing overly tight swaddling requires careful attention to technique, material selection, and infant observation. Prioritizing hip and chest freedom ensures safety and comfort.
The following section will address common misconceptions and frequently asked questions about swaddling safety and best practices.
1. Hip Dysplasia
Hip dysplasia, or developmental dysplasia of the hip (DDH), refers to a spectrum of abnormalities affecting the hip joint’s stability and alignment. A significant factor contributing to DDH involves prolonged positioning of the infant’s legs in adduction and extensionthat is, straightened and pressed together. This position directly correlates with instances where swaddling is executed too tightly, restricting natural movement. When an infant is forcibly swaddled with legs bound straight, the femoral head may be displaced from the acetabulum, the socket in the pelvis, hindering normal hip development. The impact is amplified during the first few months of life when the hip joint is most vulnerable. An overly tight swaddle transforms a potentially supportive practice into a risk factor for DDH.
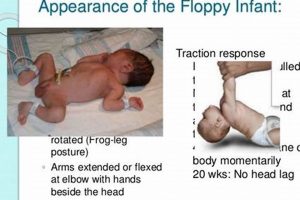
Clinical observations and research confirm the association between restrictive swaddling and increased DDH incidence. Cultures where traditional swaddling practices involve tightly binding the legs exhibit higher DDH rates. Conversely, practices that allow for hip flexion and abduction (legs bent and spread apart), often referred to as the “frog-leg” position, are considered protective. Healthcare professionals emphasize the importance of educating caregivers about safe swaddling techniques that prioritize hip health. Implementing “hip-healthy” swaddling methods is essential, particularly for infants with a family history of DDH or other risk factors. Proper swaddling can be achieved with specialized swaddle blankets designed to allow for appropriate hip movement.
Understanding the link between tight swaddling and hip dysplasia necessitates a shift towards informed care practices. Caregivers should be educated on recognizing safe swaddling positions that allow for leg movement. Continued monitoring and early detection programs are essential for identifying and addressing DDH effectively. By adopting a hip-healthy approach to swaddling, the risk of contributing to hip dysplasia can be significantly reduced, fostering optimal musculoskeletal development in infants.
2. Breathing Restriction
Swaddling practices, when executed improperly, can lead to breathing restriction in infants. This occurs when the swaddle is applied too tightly around the chest, limiting the infant’s ability to fully expand the lungs during inhalation. The consequence is reduced oxygen intake and increased respiratory effort, potentially leading to discomfort and, in severe cases, respiratory distress. The degree of restriction depends on the tightness of the swaddle and the infant’s pre-existing respiratory condition, if any.
The infant rib cage, being more cartilaginous than bone, is more pliable. A tightly bound swaddle can deform the rib cage, hindering its natural movement during breathing. For example, a caregiver may unintentionally secure the swaddle too firmly in an attempt to provide a sense of security. If an infant shows signs of rapid breathing, grunting, or retractions (pulling in of the skin between the ribs or above the sternum), this may indicate breathing difficulty due to an overly tight swaddle. A study published in Pediatrics highlighted that swaddling too tightly around the chest could reduce tidal volume, the amount of air moving in and out of the lungs, which is necessary for proper gas exchange. Parents and caregivers should be aware that swaddling must allow chest and abdominal expansion during breathing to ensure respiratory safety.
Preventing breathing restriction requires careful attention to swaddling technique. Caregivers should ensure that the swaddle allows for free movement of the chest and abdomen during respiration. Regular monitoring of the infant’s breathing pattern after swaddling is crucial. Choosing lightweight, breathable fabrics for swaddling further mitigates the risk of respiratory compromise. The ability to recognize the signs of respiratory distress early and adjust the swaddle accordingly can contribute significantly to infant safety. The significance of understanding breathing restriction as a direct consequence of improperly executed swaddling underscores the need for comprehensive education for parents and caregivers.
3. Overheating Risk
An infant’s capacity to regulate body temperature differs considerably from that of an adult. Overheating represents a significant risk, particularly when coupled with overly tight swaddling practices. A tightly wrapped infant experiences restricted airflow and reduced ability to dissipate heat effectively. The external insulation provided by multiple layers, combined with restricted movement, inhibits the body’s natural cooling mechanisms, thereby elevating the risk of hyperthermia.
Hyperthermia, induced by excessive external wrapping, can manifest in several ways. An infant may exhibit flushed skin, rapid breathing, or lethargy. These signs indicate the body is struggling to maintain a stable core temperature. Compounding the danger, overheating has been linked to an increased risk of Sudden Infant Death Syndrome (SIDS). For instance, a caregiver, acting with good intentions, may overdress and tightly swaddle an infant in a warm environment, creating conditions conducive to overheating. Conversely, loose breathable clothes and a less snug swaddle could help keep the infant’s temperature at a safe level.
Preventing overheating demands careful consideration of environmental factors, clothing choices, and swaddling technique. Caregivers should maintain a comfortable room temperature, select lightweight and breathable fabrics, and avoid overly tight swaddling. Regularly monitoring the infant for signs of overheating is crucial. By understanding the link between tight swaddling and overheating risk, caregivers can make informed decisions to prioritize infant safety and well-being, mitigating a potentially life-threatening hazard.
4. Circulation Impairment
Impaired circulation represents a potential adverse effect when swaddling infants, particularly if the technique is executed with excessive tightness. Constriction caused by overly restrictive swaddling can compromise blood flow, leading to various physiological consequences.
- Compromised Peripheral Blood Flow
Tight swaddling can exert direct pressure on blood vessels, impeding the flow of blood to the extremities. This constriction may lead to reduced blood supply to the hands and feet. If the swaddle is particularly tight around the legs, for instance, it can restrict blood flow to the feet, resulting in discoloration (paleness or blueness) or coolness to the touch. Prolonged or severe restriction could theoretically, though rarely, contribute to tissue damage. However, minor, transient instances are more common.
- Reduced Nutrient and Oxygen Delivery
Adequate blood circulation is crucial for delivering oxygen and essential nutrients to tissues. When swaddling impairs circulation, the affected areas may experience a diminished supply of these vital elements. This can affect cellular function and growth. For instance, tight swaddling around the torso may impede circulation to the abdominal organs, potentially hindering digestive processes, although such instances are difficult to isolate from other factors affecting infant digestion.
- Increased Risk of Blood Clots (Rare)
Although rare in infants, severely restricted blood flow can theoretically increase the risk of blood clot formation. Stasis of blood (slow or stagnant blood flow) provides conditions conducive to clot development. If a swaddle were to significantly impede venous return, the flow of blood back to the heart, it could potentially lead to the formation of clots in the affected area. This is an uncommon but serious potential complication, highlighting the need for caution.
- Nerve Compression and Numbness
While direct circulatory effects are the primary concern, tight swaddling can also compress nerves. Compressed nerves can manifest as tingling or numbness in the extremities, indirectly related to circulation. If the swaddle is tight around the limbs and compression of nerves occurs, this sensation would usually resolve once the swaddle is loosened or removed. This would indicate that no permanent nerve or circulatory damage has occurred.
These factors underscore the importance of employing proper swaddling techniques that avoid excessive constriction. Vigilant monitoring of the infant’s extremities for signs of circulatory compromise, such as discoloration or coolness, is crucial. Adjustments to the swaddle should be made immediately if any such signs are observed. While severe circulatory impairment from swaddling is rare, understanding the potential risks allows for proactive measures to ensure infant safety.
5. Developmental Delay
Excessively tight swaddling can inadvertently contribute to developmental delays in infants. The connection stems from the restriction of movement imposed by an overly constrictive wrap, inhibiting the infant’s ability to explore and interact with the environment. Such constrained mobility can impede the development of gross motor skills, affecting milestones such as rolling over, crawling, and eventually, walking. Early motor experiences play a critical role in shaping an infant’s understanding of their body and its capabilities. If an infant is consistently swaddled too tightly, their opportunities for spontaneous movement and exploration are diminished, potentially impacting the trajectory of motor development.
The importance of recognizing developmental delay as a potential consequence of overly tight swaddling lies in its impact on long-term outcomes. Motor skills are foundational for cognitive and social-emotional development. For example, an infant learning to reach for and grasp objects is simultaneously developing hand-eye coordination, spatial awareness, and problem-solving skills. In cases where swaddling is so restrictive that it prevents an infant from engaging in these activities, the developmental repercussions can extend beyond motor skills alone. Consider an infant consistently swaddled with their arms tightly bound; their ability to explore objects with their hands, a crucial sensory learning experience, is significantly limited. The resulting lack of sensory input may contribute to delays in cognitive development. Furthermore, an infant’s ability to self-soothe may be affected if they are unable to bring their hands to their mouth, affecting emotional regulation.
In summary, while swaddling serves a purpose in calming and promoting sleep, the potential for developmental delay as a consequence of overly tight swaddling cannot be overlooked. Ensuring proper swaddling technique, allowing for freedom of movement, and regularly assessing an infant’s motor skills are paramount. Early intervention and awareness among caregivers are crucial in mitigating the risk of developmental delays. The challenge lies in balancing the benefits of swaddling with the need for infants to freely explore and develop their motor skills, underscoring the necessity for evidence-based guidance and education.
6. Skin Irritation
Skin irritation represents a potential adverse effect stemming from improper swaddling practices. Overly tight swaddling, especially when combined with inappropriate fabric choices or inadequate hygiene, can create conditions conducive to various dermatological issues.
- Reduced Air Circulation and Trapped Moisture
Tight swaddling reduces air circulation around the infant’s skin. When the skin cannot breathe properly, moisture from sweat and natural skin secretions becomes trapped. This moist environment fosters bacterial growth and increases the risk of skin irritation. For instance, an infant swaddled in a synthetic fabric without proper ventilation may develop a heat rash or miliaria due to blocked sweat ducts. This is particularly concerning in warm climates where sweating is more pronounced. The occlusion of the skin prevents the natural shedding of dead cells and disrupts the skin barrier function. A well-ventilated, loose swaddle made from breathable materials, like cotton, can help mitigate this risk.
- Friction and Pressure Points
The pressure exerted by a tight swaddle can create friction, especially at bony prominences like elbows, knees, and shoulders. Repeated friction damages the skin’s outer layers, leading to redness, chafing, and potential abrasions. For example, an infant tightly swaddled with a rough-textured blanket may develop chafing along the skin folds. Constant pressure diminishes blood flow to the affected area, exacerbating the damage. Using soft, smooth fabrics and ensuring the swaddle is snug but not restrictive minimizes frictional irritation.
- Allergic Reactions to Fabric and Laundry Products
Infant skin is particularly sensitive to irritants and allergens. Certain fabrics, dyes, or laundry detergents can trigger allergic reactions, manifesting as skin irritation. A tightly swaddled infant is in prolonged contact with these potential allergens, increasing the likelihood of a reaction. Consider an infant who is allergic to a specific dye in a blanket; a tight swaddle concentrates the contact between the skin and the allergen, exacerbating the rash. Using hypoallergenic, fragrance-free detergents and choosing natural, dye-free fabrics minimizes the risk of allergic contact dermatitis. Thoroughly rinsing swaddling blankets removes any detergent residue that may cause irritation.
- Exacerbation of Existing Skin Conditions
Infants with pre-existing skin conditions, such as eczema or atopic dermatitis, are more susceptible to irritation from tight swaddling. The reduced air circulation, trapped moisture, and friction can worsen these conditions. For instance, an infant with eczema tightly swaddled may experience an increased flare-up of their condition, characterized by increased redness, itching, and scaling. Managing underlying skin conditions and avoiding tight swaddling prevents further irritation and complications. Choosing breathable fabrics and maintaining proper skin hydration are crucial in managing the effects of tight swaddling.
In summary, skin irritation can arise from various mechanisms related to overly tight swaddling, including reduced air circulation, friction, allergic reactions, and exacerbation of pre-existing conditions. Understanding these relationships is essential for implementing safe swaddling practices. Careful attention to fabric selection, swaddling technique, and infant hygiene is crucial in preventing skin irritation and promoting healthy skin.
Frequently Asked Questions
This section addresses common queries regarding the safe application of swaddling techniques and the potential risks associated with excessive tightness.
Question 1: What are the primary indicators that an infant is swaddled too tightly?
Indicators of an overly tight swaddle include difficulty breathing (rapid or labored), restricted movement of the limbs (particularly the hips), skin discoloration (redness or paleness) at the swaddled area, and signs of discomfort or distress exhibited by the infant (excessive crying, irritability).
Question 2: How can hip dysplasia risk be minimized when swaddling?
Hip dysplasia risk is minimized by ensuring the infant’s legs are free to flex and abduct (move apart) within the swaddle. The swaddle should allow the “frog-leg” position, where the hips and knees are bent and the legs can move outwards. Avoid swaddling the legs straight and pressed together.
Question 3: What fabrics are most suitable for swaddling to prevent overheating?
Lightweight, breathable fabrics such as cotton muslin or bamboo are most suitable. These materials promote air circulation, allowing heat to dissipate effectively and reducing the risk of overheating. Avoid synthetic fabrics that trap heat and moisture.
Question 4: At what age should swaddling be discontinued?
Swaddling should be discontinued as soon as the infant shows signs of attempting to roll over. This typically occurs around 2-4 months of age. Continuing to swaddle after the infant can roll over poses a suffocation risk, as the infant may become trapped on their stomach.
Question 5: Can overly tight swaddling affect an infant’s breathing?
Yes, an overly tight swaddle can restrict chest expansion, leading to reduced lung capacity and increased respiratory effort. This is particularly dangerous for infants with pre-existing respiratory conditions.
Question 6: How often should the tightness of the swaddle be checked?
The tightness of the swaddle should be checked regularly, at least every hour, especially during the initial learning phase of swaddling. Additionally, the swaddle should be re-evaluated after feeding or changes in the infant’s activity level.
Proper swaddling technique balances security and freedom, prioritizing the infant’s respiratory and musculoskeletal health. Vigilant monitoring remains crucial for ensuring safety.
The subsequent section will summarize the key points of the article and provide a concise set of guidelines for safe swaddling practices.
Can You Swaddle a Baby Too Tight?
The preceding discussion has addressed the pertinent question: can you swaddle a baby too tight? Overly restrictive swaddling carries potential risks, including hip dysplasia, breathing restriction, overheating, circulation impairment, developmental delay, and skin irritation. Proper swaddling technique necessitates a balance between security and freedom of movement, particularly allowing for hip flexion and chest expansion. Vigilant monitoring of the infant’s breathing, skin condition, and overall comfort remains essential. Appropriate fabric selection and environmental considerations further contribute to safe swaddling.
Safe swaddling practices are not merely a matter of technique but are directly linked to infant well-being. Caregivers should remain informed and proactive in adapting their approach to meet the evolving needs of the developing infant. Continuous education and consultation with healthcare professionals are critical to ensure that swaddling remains a safe and beneficial practice.