The query addresses a common parental concern: whether infants experience a reduction in food intake during the eruption of their teeth. This potential decrease in appetite is often attributed to discomfort and inflammation in the gums. Parents frequently observe changes in their child’s feeding habits during periods associated with tooth emergence.
Understanding the correlation between dental development and feeding patterns is significant for ensuring adequate nutrition and managing parental anxieties. Historically, teething has been associated with various symptoms, some accurately and others based on anecdotal evidence. Recognizing the actual impact on nutritional intake allows for appropriate interventions and prevents unnecessary medical consultations.
The following discussion will explore the physiological reasons why infants might exhibit altered eating behaviors while their teeth are erupting, differentiate between typical teething symptoms and those indicative of other underlying illnesses, and provide strategies for maintaining adequate nourishment during this developmental stage.
Strategies for Nutritional Maintenance During Teething
When dental development coincides with reduced food consumption, implementing specific strategies can help ensure infants receive adequate nourishment and minimize discomfort.
Tip 1: Offer Soft Foods. Purees, yogurt, and applesauce require minimal chewing and are less likely to irritate inflamed gums.
Tip 2: Serve Cold Items. Chilled foods and beverages can provide a soothing, numbing effect that alleviates gum pain. A cooled teether can also be offered before meals.
Tip 3: Divide Meals into Smaller, More Frequent Portions. Rather than adhering to a rigid feeding schedule, offer smaller amounts of food more often throughout the day. This may increase overall intake.
Tip 4: Consider Pain Relief. If discomfort is significant, consulting a pediatrician regarding appropriate pain relief options, such as acetaminophen or ibuprofen, is advisable. Use these medications as directed by a healthcare professional.
Tip 5: Gently Massage Gums. Before feeding, lightly massaging the infant’s gums with a clean finger or a soft, damp cloth can provide temporary relief and potentially encourage greater acceptance of food.
Tip 6: Maintain Hydration. Ensure adequate fluid intake, especially if solid food consumption is reduced. Water or diluted fruit juice can help prevent dehydration.
Tip 7: Avoid Sugary Foods and Drinks. Sugar can exacerbate gum inflammation and contribute to dental caries. Opt for naturally sweet foods like fruits and vegetables.
Employing these methods can assist in maintaining adequate nutrient intake, easing discomfort, and supporting healthy growth throughout the teething process.
The subsequent section will address distinguishing teething symptoms from those indicative of more serious medical conditions.
1. Discomfort and Inflammation
The presence of oral discomfort and gingival inflammation during tooth eruption is a primary factor influencing an infant’s feeding behavior. These physiological responses to teething can directly affect an infant’s willingness and ability to consume food, potentially leading to a reduction in food intake.
- Gingival Sensitivity
Erupting teeth cause inflammation of the gingival tissues, resulting in increased sensitivity to pressure and touch. This heightened sensitivity can make the act of chewing and sucking painful, discouraging the infant from engaging in these behaviors. The introduction of solid foods, which require more vigorous chewing, may be particularly problematic during periods of intense gingival sensitivity. Even breastfeeding or bottle-feeding can become uncomfortable due to the pressure exerted on the gums.
- Local Inflammatory Response
The body’s natural inflammatory response to tooth eruption involves the release of inflammatory mediators in the gum tissue. These substances contribute to swelling, redness, and increased temperature in the affected area. While this response is a normal part of the teething process, it can cause significant discomfort and irritability in the infant. Systemic effects such as mild fever may accompany the local inflammation. The overall discomfort experienced by the infant may manifest as a decreased appetite.
- Pain Perception
The eruption of teeth stimulates sensory nerve endings in the gums, transmitting pain signals to the brain. The intensity of pain experienced varies among infants, but persistent or acute pain can significantly impact feeding behavior. An infant may associate feeding with pain, leading to a reluctance to eat. The experience of pain can also disrupt sleep patterns, further contributing to irritability and decreased appetite.
- Textural Aversion
Inflamed and sensitive gums can alter an infant’s perception of food textures. Foods that were previously accepted may become irritating due to their consistency. For example, coarse or hard foods may exacerbate gum discomfort, leading to a preference for smoother, softer textures. This textural aversion can limit the variety of foods an infant is willing to consume, potentially impacting nutritional intake.
In summary, the discomfort and inflammation associated with tooth eruption create a complex interplay of physiological and behavioral responses that can significantly affect an infant’s feeding patterns. Heightened gingival sensitivity, local inflammatory responses, pain perception, and textural aversions all contribute to a potential reduction in food intake. Monitoring these factors and implementing appropriate strategies to mitigate discomfort is essential for maintaining adequate nutrition during this developmental phase.
2. Altered Food Preferences
The eruption of teeth can precipitate discernible shifts in an infant’s predilection for certain foods. This alteration in preference constitutes a significant element in the phenomenon of reduced food intake during teething. The physical discomfort experienced during tooth emergence may lead infants to reject previously accepted food textures, temperatures, or flavors, resulting in a narrower range of palatable options. For instance, an infant who readily consumed mashed vegetables may suddenly refuse them, exhibiting a preference only for smoother purees or liquids. This change stems from the increased sensitivity in the gums, making the chewing or swallowing of certain consistencies unpleasant. The importance of recognizing these altered preferences lies in the ability to adapt feeding strategies to maintain adequate nutrition, albeit through modified means.
Practical application of this understanding involves careful observation of an infant’s reactions to different foods during teething periods. If a rejection of certain foods is noted, temporary substitution with alternatives of similar nutritional value but differing texture or temperature is warranted. For example, if warm foods cause discomfort, serving chilled or room-temperature alternatives may improve acceptance. Similarly, if an infant refuses solid foods, increasing the proportion of liquid-based meals, such as yogurt or fruit smoothies, can help maintain caloric intake. These adjustments require a proactive and responsive approach to feeding, tailored to the individual infant’s changing needs and preferences. These changes in the baby, is crucial.
In summation, altered food preferences represent a key factor contributing to the reduction in food consumption observed during the teething process. The physical discomfort experienced influences an infant’s willingness to accept certain foods, necessitating adjustments in feeding strategies to ensure adequate nutrition. Early identification and adaptive feeding practices are crucial for mitigating the impact of altered preferences, ultimately supporting healthy growth and development during this phase. These adjustments should be done gradually and patiently to help babies.
3. Gum Sensitivity
Gum sensitivity is a primary etiological factor in diminished food consumption during the teething process. The emergence of teeth through the gingival tissues triggers an inflammatory response, resulting in heightened sensitivity to pressure and tactile stimulation. This increased sensitivity directly impacts the infant’s willingness to engage in feeding, as the act of chewing or sucking exacerbates discomfort. For example, an infant previously amenable to consuming solid foods may exhibit reluctance or refusal due to the increased pressure on inflamed gums during mastication. Similarly, even the gentle pressure of a nipple during breastfeeding or bottle-feeding can induce discomfort, leading to reduced intake and shorter feeding sessions. The degree of sensitivity varies between individuals and can fluctuate throughout the teething period, thereby influencing the variability in feeding patterns.
Practical implications of understanding the connection between gum sensitivity and decreased food intake involve adapting feeding strategies to minimize discomfort. Offering softer foods that require minimal chewing, such as purees or yogurt, can reduce the pressure on sensitive gums. Chilling foods or offering cold teething rings prior to meals may provide a numbing effect, temporarily alleviating pain. Additionally, smaller, more frequent feedings can be less overwhelming than large meals, allowing the infant to consume nutrients without prolonged pressure on the gums. Parents and caregivers should also be vigilant in observing signs of increased sensitivity, such as fussiness during feeding or resistance to certain textures, and adjust accordingly. In cases of severe discomfort, consultation with a pediatrician regarding appropriate analgesics may be warranted.
In summary, gum sensitivity represents a significant contributing factor to the observed reduction in food intake during teething. The inflammatory response and heightened tactile sensitivity associated with tooth eruption create a barrier to comfortable and effective feeding. By recognizing this connection and implementing adaptive feeding strategies, caregivers can mitigate discomfort and ensure adequate nutritional intake throughout the teething phase. Addressing gum sensitivity directly is essential for maintaining optimal growth and development during this critical period of infant development.
4. Feeding Frequency
During teething, alterations in feeding frequency often accompany a decrease in overall food consumption. Discomfort associated with tooth eruption can lead to shorter, more frequent feeding sessions as infants may become easily agitated or overwhelmed by prolonged sucking or chewing. This change in feeding behavior is a direct response to the pain and inflammation experienced in the gums, causing them to seek shorter intervals of relief between feeds. Consequently, adherence to previously established feeding schedules may become challenging, requiring caregivers to adopt a more flexible approach tailored to the infants comfort level. For instance, an infant who typically nurses every three to four hours might demand smaller, more frequent feeds every one to two hours during a teething episode. This shift is not necessarily indicative of increased hunger but rather a strategy to minimize prolonged discomfort. The significance of recognizing this shift lies in the ability to adapt feeding practices to meet the infant’s needs without forcing them to endure extended periods of oral discomfort.
The practical implication of this understanding involves a responsive feeding approach, where caregivers closely observe the infant’s cues and adjust feeding frequency accordingly. Rather than adhering rigidly to a set schedule, caregivers should offer smaller, more frequent meals or nursing sessions, catering to the infants comfort and willingness to feed. For example, if an infant refuses a full bottle at the usual feeding time, offering a smaller amount more frequently throughout the day can help maintain adequate caloric intake without exacerbating discomfort. This approach requires patience and attentiveness, as it may involve more frequent interruptions to the caregiver’s routine. Additionally, offering soothing measures, such as chilled teething toys or gentle gum massage, before feeding can help alleviate discomfort and potentially encourage greater intake during these more frequent sessions. Understanding the importance of the baby’s condition is a must.
In summary, changes in feeding frequency are intrinsically linked to decreased food consumption during teething. Discomfort-driven alterations in feeding behavior necessitate a flexible and responsive feeding approach, emphasizing smaller, more frequent sessions tailored to the infant’s comfort level. By recognizing and adapting to these changes, caregivers can effectively mitigate discomfort, maintain adequate nutritional intake, and support healthy growth and development throughout the teething process. This approach should be observed carefully to avoid overfeeding, and if weight changes are concerning, consulting a healthcare professional is recommended.
5. Nutritional Adequacy
Nutritional adequacy, defined as the sufficient intake of essential nutrients to support growth and development, is intrinsically linked to feeding patterns observed during periods of tooth eruption. The commonly reported reduction in food intake associated with teething raises concerns regarding the maintenance of adequate nutrition during this developmental stage. If an infant consistently consumes less food due to teething discomfort, the risk of nutrient deficiencies increases, potentially impacting overall health and growth trajectory. For example, reduced iron intake can lead to iron-deficiency anemia, while insufficient calcium and vitamin D can compromise bone development. Therefore, the extent to which an infant’s food intake is diminished during teething and the duration of this altered feeding behavior directly influence nutritional status.
Addressing the potential compromise in nutritional adequacy requires proactive monitoring and adaptive strategies. Regular weight checks and observation of developmental milestones can provide indicators of nutritional status. Implementing strategies such as offering softer, more palatable foods, adjusting feeding frequency, and considering appropriate pain relief measures are critical in mitigating the impact of reduced intake. In cases where dietary modifications are insufficient, consultation with a pediatrician or registered dietitian is warranted to assess the need for supplemental nutrients. Early intervention is essential to prevent the development of nutrient deficiencies and ensure that the infant receives the necessary building blocks for optimal growth and development.
In summary, the intersection of reduced food intake during teething and the maintenance of nutritional adequacy presents a significant consideration in infant care. While some reduction in intake may be transient and inconsequential, prolonged or severe alterations in feeding patterns can jeopardize nutritional status. Vigilant monitoring, adaptive feeding strategies, and timely intervention are crucial to safeguarding nutritional adequacy and supporting healthy growth and development during periods of tooth eruption. Failing to address this potential compromise can have long-term implications for the infant’s health and well-being.
6. Underlying Conditions
The potential for underlying medical conditions to mimic or exacerbate teething symptoms necessitates careful differentiation to ensure appropriate management. While decreased appetite is commonly attributed to teething, various illnesses can manifest similarly, complicating the diagnostic process. For instance, an ear infection, characterized by inflammation and discomfort, may lead to irritability and reduced feeding, overlapping with typical teething symptoms. Similarly, gastrointestinal issues, such as viral or bacterial infections, can cause nausea and loss of appetite, further blurring the lines between teething and illness. Allergic reactions, particularly those affecting the oral cavity, can also contribute to feeding aversion. Consequently, assuming that a decline in food intake is solely due to teething without considering alternative diagnoses can delay necessary medical intervention, potentially leading to adverse outcomes.
Differentiating teething from underlying conditions requires a comprehensive assessment that includes a detailed medical history, physical examination, and consideration of associated symptoms. The presence of fever above 101F (38.3C), persistent diarrhea, vomiting, rash, or lethargy suggests a cause beyond teething and necessitates prompt medical evaluation. Additionally, observing the infant’s overall behavior, such as responsiveness to stimuli and level of activity, can provide further clues. If uncertainty persists, diagnostic testing, such as blood work or stool analysis, may be required to rule out infections or other medical conditions. The accurate identification of the underlying cause is critical for initiating appropriate treatment and preventing complications. For example, misattributing a urinary tract infection to teething can lead to delayed antibiotic therapy and potential kidney damage.
In summary, the potential for underlying conditions to mimic or exacerbate teething symptoms underscores the importance of a thorough diagnostic approach. While reduced food intake is a common complaint during teething, other illnesses must be considered and ruled out through careful assessment and, if necessary, diagnostic testing. Accurately differentiating teething from underlying medical conditions ensures timely and appropriate intervention, preventing delays in treatment and safeguarding the infant’s overall health and well-being. Dismissing concerning symptoms as “just teething” can have serious consequences, highlighting the need for vigilance and a commitment to comprehensive evaluation.
Frequently Asked Questions
This section addresses common inquiries regarding infant feeding patterns during the teething process, providing evidence-based information to aid caregivers.
Question 1: Is a decrease in appetite a normal occurrence during teething?
A transient reduction in appetite is frequently observed during tooth eruption. The associated gum inflammation and discomfort can temporarily diminish an infant’s willingness to consume food.
Question 2: Are all instances of decreased appetite attributable to teething?
Not all instances of reduced food intake should be attributed solely to teething. Underlying medical conditions, such as infections or allergies, can also manifest as decreased appetite. Careful assessment is warranted to rule out alternative causes.
Question 3: What feeding strategies can be implemented to mitigate reduced food intake during teething?
Strategies include offering softer foods, serving chilled items, providing smaller, more frequent meals, and considering appropriate pain relief measures, as directed by a healthcare professional.
Question 4: How can one differentiate between typical teething symptoms and signs of a more serious illness?
Signs such as high fever (above 101F or 38.3C), persistent diarrhea, vomiting, rash, or lethargy are not typical of teething and warrant prompt medical evaluation.
Question 5: Is there a specific age range during which teething-related appetite changes are most likely to occur?
Teething-related appetite changes are most commonly observed between 6 and 24 months of age, coinciding with the typical period of primary tooth eruption.
Question 6: When should a healthcare professional be consulted regarding feeding concerns during teething?
A healthcare professional should be consulted if the decrease in appetite is prolonged, significant weight loss occurs, or if other concerning symptoms are present.
Key takeaways include the understanding that reduced appetite is a common but not universal symptom of teething, and that careful monitoring and adaptive feeding strategies can help ensure adequate nutrition during this developmental phase.
The following section will provide a summary of the key considerations discussed throughout this article.
Do Babies Eat Less When Teething
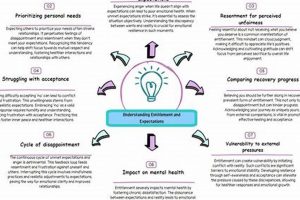
The exploration of whether infants exhibit reduced food intake during the teething process reveals a complex interplay of physiological and behavioral factors. Gum inflammation, discomfort, altered food preferences, and changes in feeding frequency can all contribute to a temporary decrease in appetite. However, it is crucial to recognize that not all instances of reduced feeding are attributable solely to tooth eruption, and underlying medical conditions must be considered.
Vigilant monitoring of feeding patterns, adaptive strategies to mitigate discomfort, and differentiation from other illnesses are essential for ensuring adequate nutritional intake during this developmental stage. A proactive and informed approach, coupled with timely consultation with healthcare professionals when concerns arise, will safeguard infant health and well-being throughout the teething process and beyond.