These items represent a thoughtful approach to infant comfort, integrating superior materials and construction with custom design elements. An example would be a soft, breathable blanket made of organic cotton, embroidered with a child’s name and birthdate.
Such creations offer significant value, providing a safe and comfortable environment for infants while also serving as cherished keepsakes. Their history is rooted in the tradition of hand-crafted gifts, evolving to incorporate modern manufacturing techniques and personalization options that enhance their sentimental worth.
Subsequent sections will delve into the materials commonly used, the various personalization techniques available, and the factors to consider when selecting the ideal item for a child.
Guidance on Selecting Customized Infant Wraps
The following outlines key considerations when acquiring customized infant wraps, emphasizing superior craftsmanship and personalized features.
Tip 1: Material Selection. Prioritize natural, hypoallergenic fabrics such as organic cotton or bamboo. These minimize potential skin irritation and ensure breathability for the infant.
Tip 2: Stitching and Construction. Examine the quality of the stitching. Tight, even seams indicate durability and prevent fraying, extending the lifespan of the item.
Tip 3: Personalization Method. Consider the longevity and aesthetic appeal of the personalization technique. Embroidery offers a classic, enduring look, while dye-sublimation provides vibrant, detailed images that resist fading.
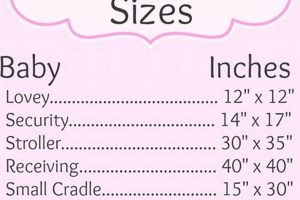
Tip 4: Size and Dimensions. Select a size appropriate for the infant’s current age and anticipated growth. A larger blanket offers versatility for swaddling, tummy time, and stroller use.
Tip 5: Safety Certifications. Ensure the item meets relevant safety standards, such as Oeko-Tex certification, which verifies the absence of harmful chemicals.
Tip 6: Washability and Care. Opt for machine-washable options for convenient cleaning. Follow the manufacturer’s instructions to maintain the fabric’s integrity and prevent shrinkage or fading.
Tip 7: Design Coherence. Align the personalized design elements with the overall aesthetic of the nursery or gifting theme. Consider font styles, color palettes, and image resolution for a cohesive result.
Adhering to these guidelines ensures a purchase that balances aesthetic appeal with infant safety and long-term usability.
The subsequent section will summarize the various avenues through which these specialized items can be acquired.
1. Material composition
Material composition is a foundational determinant of the quality and suitability of customized infant coverings. The chosen materials directly influence the item’s safety, comfort, durability, and overall value. Therefore, a meticulous evaluation of material properties is essential.
- Fiber Type
The fiber typenatural, synthetic, or blendeddictates the tactile feel, breathability, and potential for allergic reactions. Natural fibers like organic cotton and bamboo are often preferred due to their inherent softness and hypoallergenic properties. Synthetic fibers, while potentially more durable, may lack breathability and can cause skin irritation in sensitive infants. The selection of fiber type represents a fundamental trade-off between comfort, durability, and cost.
- Fabric Construction
The manner in which fibers are woven or knitted together significantly affects the blanket’s texture, drape, and thermal properties. Tightly woven fabrics offer increased durability and wind resistance, while loosely knitted fabrics provide greater breathability and a softer feel. The choice of fabric construction depends on the intended use and the desired balance between warmth and ventilation. For instance, a tightly woven cotton flannel is suitable for colder climates, whereas a loosely knitted muslin is preferable for warmer conditions.
- Dye and Treatment Processes
The dyes and treatments applied to the fabric during manufacturing can have significant implications for infant health and safety. Harsh chemicals and dyes may cause skin irritation, allergic reactions, or even pose more serious health risks. The use of low-impact dyes and non-toxic treatments is paramount. Certifications such as Oeko-Tex Standard 100 provide assurance that the fabric has been tested for harmful substances and meets stringent safety standards.
- Weight and Thickness
The weight and thickness of the fabric influence its warmth, drape, and overall bulk. A heavier, thicker fabric provides greater insulation, while a lighter, thinner fabric is more breathable and easier to manage. The optimal weight and thickness depend on the climate and the infant’s individual needs. A lightweight muslin is suitable for swaddling in warm weather, while a heavier fleece is more appropriate for colder environments.
In conclusion, material composition is not merely a superficial attribute but a critical determinant of the utility and value of infant coverings. Each component, from fiber selection to processing methods, contributes to the item’s performance and safety. Careful consideration of these factors ensures that the final product meets the stringent requirements for infant care.
2. Manufacturing excellence
Manufacturing excellence, in the context of superior infant coverings, refers to the rigorous standards and precise processes employed throughout production. It directly impacts the product’s durability, safety, and aesthetic appeal. Without stringent quality control measures, even the finest materials may be rendered substandard.
- Seam Integrity
Precise and durable seam construction is critical for preventing unraveling and ensuring the product withstands repeated use and laundering. Weak or poorly executed seams represent a safety hazard, potentially exposing infants to loose threads. Examples of superior seam construction include reinforced stitching and serged edges, common in high-end baby blankets. The implications of poor seam integrity extend beyond aesthetics; it directly impacts the longevity and safety of the product.
- Embroidery Precision
For personalized elements, the accuracy and consistency of embroidery are paramount. Misaligned lettering, uneven stitch density, or color bleeding detract from the overall aesthetic and indicate a lack of attention to detail. High-quality personalized items exhibit crisp, clean embroidery, utilizing durable threads resistant to fading. Such precision reflects a commitment to craftsmanship and enhances the perceived value of the item.
- Material Cutting and Alignment
Accurate cutting and alignment of fabric panels are essential for ensuring proper fit and symmetry. Skewed patterns or uneven edges demonstrate inadequate quality control measures. Manufacturing excellence dictates that each panel is precisely cut and aligned, resulting in a visually appealing and structurally sound product. This level of precision requires skilled operators and advanced cutting technologies.
- Finishing Details
Attention to finishing details, such as thread trimming, label placement, and packaging, contributes to the overall perception of quality. Loose threads, crooked labels, or damaged packaging detract from the product’s appeal. Manufacturing excellence encompasses a meticulous approach to these details, ensuring that the final product is presented in a pristine and professional manner. Such attention reinforces the brand’s commitment to quality and customer satisfaction.
In summary, manufacturing excellence is not merely an abstract concept but a tangible attribute reflected in every aspect of the product. From seam integrity to finishing details, each element contributes to the overall quality and value. Items crafted with manufacturing excellence not only provide comfort and warmth but also serve as enduring keepsakes, reflecting the care and attention invested in their creation.
3. Personalization Longevity
Personalization longevity is a crucial factor when evaluating customized infant textiles. The endurance of personalized elements directly contributes to the item’s sentimental value and its ability to serve as a lasting keepsake. Deterioration of these elements diminishes the intended impact and reduces the overall worth of the product.
- Thread Durability
The type and quality of thread used for embroidery or appliqu significantly influence the longevity of personalized details. Inferior threads are prone to fading, fraying, or breaking after repeated washing, compromising the clarity and integrity of the design. For high-quality items, colorfast and durable threads, such as those made from polyester or rayon, are employed to ensure the personalization remains vibrant and intact over time.
- Application Technique
The method used to apply personalized elements affects their resistance to wear and tear. Heat-transfer vinyl, while offering detailed designs, may crack or peel with frequent washing. Embroidery, with its stitched construction, provides a more durable and permanent solution. Dye-sublimation, where the ink is infused directly into the fabric fibers, also offers excellent longevity and resistance to fading. The choice of application technique represents a trade-off between cost, detail, and durability.
- Fabric Stability
The stability of the base fabric plays a role in preserving the integrity of personalized elements. If the fabric shrinks excessively or distorts during washing, it can cause puckering or distortion of embroidered or appliqud designs. High-quality items utilize pre-shrunk fabrics and stable weaves to minimize dimensional changes and maintain the original appearance of the personalization. This is particularly important for items intended to be washed frequently.
- UV Resistance
Exposure to ultraviolet (UV) radiation can cause fading and discoloration of both the fabric and the personalized elements. This is particularly relevant for items that will be used outdoors, such as stroller blankets. High-quality items utilize UV-resistant dyes and fabrics to minimize the effects of sun exposure and maintain the vibrancy of the personalization. This is often achieved through specialized fabric treatments or the selection of inherently UV-resistant fibers.
The interconnectedness of thread durability, application technique, fabric stability, and UV resistance underscores the importance of holistic material and process selection. The longevity of personalized elements is not solely determined by a single factor but by the synergistic effect of multiple variables. A failure in any of these areas can compromise the overall value and sentimental worth of the item.
4. Infant safety
Infant safety is a paramount consideration in the design and manufacture of customized infant coverings. The materials, construction, and personalization methods employed must adhere to rigorous safety standards to minimize potential hazards.
- Material Toxicity
The use of non-toxic materials is critical to prevent infants from exposure to harmful chemicals through skin contact or ingestion. Fabrics and dyes must be free from substances such as lead, phthalates, and formaldehyde, which can pose serious health risks. Reputable manufacturers prioritize certified organic cotton and low-impact dyes to ensure the safety of their products. For example, a baby blanket with high levels of formaldehyde can lead to skin irritation and respiratory problems.
- Suffocation Hazards
Loose threads, ribbons, or appliqus can present suffocation hazards for infants. High-quality infant coverings are constructed with secure seams and minimal embellishments to reduce the risk of entanglement or ingestion. Blankets should also be appropriately sized to prevent them from covering the infant’s face during sleep. The omission of small, detachable parts, is a critical safety measure that needs to be taken.
- Flammability
Infant textiles must meet stringent flammability standards to protect infants from burns in the event of a fire. Materials should be inherently flame-resistant or treated with non-toxic flame retardants. Compliance with relevant safety regulations, such as the Consumer Product Safety Improvement Act (CPSIA), is essential. A highly flammable material used in a blanket could endanger the infants safety if exposed to a heat source.
- Allergenicity
Certain materials can trigger allergic reactions in sensitive infants. Common allergens include synthetic fibers, dyes, and chemical treatments. High-quality infant coverings utilize hypoallergenic materials, such as organic cotton or bamboo, and avoid the use of harsh chemicals to minimize the risk of allergic reactions. Thorough washing before first use can further reduce the presence of potential irritants. Ensuring that the materials are allergen-free is imperative for safeguarding the infants health.
These considerations highlight the importance of prioritizing infant safety when selecting customized infant coverings. Opting for products from reputable manufacturers who adhere to stringent safety standards is essential for protecting the well-being of infants. The intersection of high-quality materials, safe construction, and thoughtful personalization creates an item that provides comfort and minimizes potential risks.
5. Design uniqueness
Design uniqueness, in the context of superior, customized infant wraps, signifies a departure from standardized offerings. It elevates the product from a mere functional item to a bespoke keepsake, reflecting individual preferences and sentimental value. The following facets illuminate this concept.
- Original Motif Development
The creation of original motifs, rather than reliance on generic templates, distinguishes high-quality personalized items. This involves commissioning original artwork, graphic design, or custom embroidery patterns. An example would be a blanket featuring a hand-drawn illustration of the recipient’s favorite animal or a custom-designed monogram. This investment in original design elements elevates the perceived value and aesthetic appeal of the item.
- Color Palette Harmonization
A carefully considered color palette enhances the visual appeal and emotional resonance of the item. The selection of colors should complement the infant’s nursery decor or reflect the recipient’s personal style. Examples include the use of complementary colors to create visual interest or the incorporation of pastel shades to evoke a sense of calm and serenity. This attention to color harmony contributes to the overall sophistication and aesthetic quality of the product.
- Typographic Integration
The selection and integration of typography play a crucial role in conveying the intended message and enhancing the visual impact of personalized text. The font style, size, and placement should be carefully considered to ensure legibility and aesthetic coherence. Examples include the use of elegant calligraphy fonts for formal occasions or playful sans-serif fonts for casual settings. The integration of typography should be seamless and contribute to the overall design aesthetic.
- Material Texture Contrast
The strategic use of contrasting textures can enhance the tactile and visual appeal of the item. This involves combining different fabrics or embellishments to create a multi-sensory experience. Examples include the juxtaposition of smooth satin with textured knit or the incorporation of raised embroidery for added dimension. This attention to tactile detail elevates the sensory experience and adds a layer of sophistication to the design.
These interconnected elements of original motif development, color palette harmonization, typographic integration, and material texture contrast collectively contribute to design uniqueness. High-quality, customized infant wraps that prioritize these elements transcend mere functionality, becoming cherished keepsakes that embody individual expression and enduring value. Design uniqueness offers a substantial upgrade to an otherwise utilitarian product.
Frequently Asked Questions
This section addresses common inquiries regarding the selection, care, and safety of customized infant coverings, providing clarity and guidance for discerning consumers.
Question 1: What materials are most suitable for infant wraps intended for sensitive skin?
Organic cotton and bamboo are generally recommended for infants with sensitive skin due to their hypoallergenic properties and absence of harsh chemicals. These materials minimize the risk of irritation and promote breathability.
Question 2: How can the durability of personalized embroidery be ensured?
The use of high-quality, colorfast threads, coupled with a tight stitch density, enhances the longevity of embroidered personalization. Washing the item inside-out and avoiding harsh detergents can further preserve the design’s integrity.
Question 3: What safety certifications should consumers look for when purchasing these items?
Certifications such as Oeko-Tex Standard 100 indicate that the product has been tested for harmful substances and meets stringent safety standards. These certifications provide assurance of product safety and quality.
Question 4: How does the weight of the blanket impact its suitability for different climates?
Lighter-weight materials, such as muslin or cotton voile, are preferable for warmer climates, while heavier materials, such as fleece or flannel, offer greater insulation in colder climates. The appropriate weight depends on the ambient temperature and the infant’s individual needs.
Question 5: What cleaning methods are recommended for preserving the quality of personalized items?
Machine washing in cold water with a mild detergent is generally recommended. Avoid using bleach or fabric softeners, as these can damage the fabric and fade the personalized details. Tumble drying on low heat or air drying is preferable.
Question 6: How can the risk of suffocation be minimized when using infant wraps?
Blankets should be appropriately sized and avoid excessive embellishments, such as ribbons or loose threads, that could pose a suffocation hazard. Supervise infants when using blankets and avoid placing them directly in the crib with the infant during sleep.
These FAQs offer a comprehensive overview of the factors to consider when acquiring superior, customized infant wraps. Prioritizing material safety, construction quality, and personalization longevity ensures a valuable and cherished keepsake.
The subsequent section will provide resources for locating reputable suppliers of high-quality personalized baby blankets.
Conclusion
This exploration has elucidated the multifaceted considerations inherent in acquiring high quality personalized baby blankets. The discussion encompassed material composition, manufacturing excellence, personalization longevity, infant safety, and design uniqueness. Each element contributes critically to the overall value and suitability of these items as both functional necessities and cherished keepsakes.
Given the potential impact on infant well-being and the enduring sentimental value, meticulous evaluation and discerning selection are paramount. A commitment to quality and safety ensures that these investments provide comfort, security, and lasting memories. Further research into reputable suppliers and adherence to recommended care practices will optimize the longevity and utility of these personalized items.