Specialized infant nutrition products are designed to alleviate the symptoms of persistent and excessive crying in infants, often associated with digestive discomfort. These formulations often incorporate partially hydrolyzed proteins, reduced lactose content, and added prebiotics to improve digestion and gut health in susceptible babies. For instance, some products contain whey protein that has been broken down into smaller peptides, making it easier for the infant to digest.
The development and use of these specialized products address a significant concern for parents and healthcare providers. They aim to provide nutritional support while reducing the frequency and intensity of crying episodes, improving both infant comfort and parental well-being. Historically, such products represent an evolution in infant nutrition, reflecting a growing understanding of the relationship between diet and infant gastrointestinal distress. This evolution considers improved digestive comfort and reduced crying.
This article will delve into the specific ingredients commonly found in these specialized products, explore the scientific evidence supporting their effectiveness, and provide guidance on selecting and using them appropriately under the guidance of healthcare professionals. The subsequent sections will analyze the components, efficacy, and safe usage of these options.
Guidance on the Selection and Use of Specialized Infant Nutrition
The selection and utilization of specialized infant nutrition requires careful consideration. Parents and caregivers should consult with pediatricians or healthcare providers to determine the appropriateness of such products for their infant.
Tip 1: Consult a Healthcare Professional: Prior to initiating any change in an infant’s diet, seek advice from a pediatrician or registered dietitian. They can assess the infant’s specific needs and provide tailored recommendations.
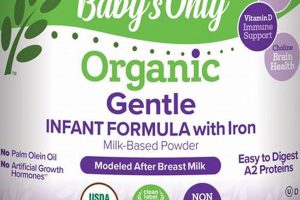
Tip 2: Understand Ingredient Composition: Scrutinize the product label, paying close attention to the protein source (e.g., hydrolyzed whey), carbohydrate content (e.g., reduced lactose), and presence of prebiotics or probiotics. Understanding the specific components can aid in assessing suitability for the infant.
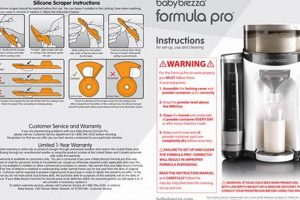
Tip 3: Follow Preparation Instructions Meticulously: Adhere precisely to the preparation instructions provided by the manufacturer. Incorrect mixing ratios or temperatures can compromise the nutritional value and safety of the product.
Tip 4: Monitor Infant’s Response: Closely observe the infant for any changes in behavior, feeding patterns, or stool consistency following the introduction of the specialized nutrition. Report any adverse reactions to a healthcare provider.
Tip 5: Introduce Gradually: When transitioning from a standard to a specialized nutrition product, consider doing so gradually to minimize potential digestive upset. This may involve mixing the two products in increasing proportions over several days.
Tip 6: Ensure Proper Storage: Store the product in accordance with the manufacturer’s guidelines, typically in a cool, dry place. Discard any opened containers after the recommended period to maintain product quality and safety.
Tip 7: Consider Potential Allergens: Be mindful of potential allergens present in the product, particularly if the infant has a known history of food allergies or sensitivities. Read labels carefully and consult with a healthcare provider if concerns arise.
Adherence to these guidelines supports informed decision-making when considering the use of specialized infant nutrition, promoting optimal infant health and well-being.
The subsequent sections will delve into the potential benefits and limitations of various specialized nutrition options, providing a balanced perspective on their role in infant care.
1. Hydrolyzed Proteins
Hydrolyzed proteins constitute a core component of specialized infant formulas designed to mitigate the symptoms of colic. The rationale for their inclusion stems from the understanding that some infants experience difficulty digesting intact proteins, particularly cow’s milk proteins. This incomplete digestion can lead to gastrointestinal distress, contributing to the excessive crying and discomfort characteristic of colic. Hydrolyzed proteins, by contrast, are proteins that have been broken down into smaller peptides and amino acids, effectively pre-digesting them. This reduced size facilitates easier and more complete digestion, lessening the burden on the infant’s immature digestive system. Consequently, hydrolyzed proteins diminish the likelihood of triggering an inflammatory response or allergic reaction in susceptible infants.
Real-world examples frequently demonstrate the effectiveness of hydrolyzed protein formulas in reducing colic symptoms. For instance, infants who consistently cried excessively and displayed signs of discomfort after feeding with standard cow’s milk-based formulas often exhibited a significant decrease in crying duration and improved comfort levels after being switched to a formula containing partially or extensively hydrolyzed proteins. Studies have shown that partially hydrolyzed formulas may be adequate for some infants, while others may require extensively hydrolyzed formulas, where the proteins are broken down into even smaller components, particularly if the infant has a known cow’s milk protein allergy or sensitivity. However, the practical significance lies in the personalized approach to selecting the appropriate level of protein hydrolysis, often guided by a healthcare professional’s assessment of the infant’s specific needs and symptoms.
In summary, hydrolyzed proteins play a pivotal role in specialized infant formulas by promoting easier digestion and reducing the potential for gastrointestinal distress. While not a panacea for all causes of colic, the inclusion of hydrolyzed proteins addresses a significant contributing factor, potentially alleviating symptoms and improving infant comfort. The appropriate selection of a hydrolyzed protein formula, guided by healthcare professional, is critical to maximizing its benefits and ensuring optimal infant health. However, challenges may arise in determining the underlying cause of colic, necessitating a comprehensive diagnostic approach to rule out other potential medical conditions.
2. Reduced Lactose
Reduced lactose content is a notable modification in some infant formulas designed to mitigate symptoms of colic, particularly in infants exhibiting signs of lactose intolerance or sensitivity. The rationale behind this adjustment lies in the potential for undigested lactose to contribute to gastrointestinal distress.
- Mechanism of Action
Lactose, a disaccharide found in milk, requires the enzyme lactase for proper digestion. In infants with lactase deficiency or reduced lactase activity, undigested lactose ferments in the colon, leading to gas production, bloating, and abdominal discomfort. Reducing the lactose content in infant formula aims to minimize this fermentation process and alleviate associated symptoms.
- Clinical Manifestations
The clinical benefits of reduced-lactose formulas are primarily observed in infants who display colic-like symptoms, such as excessive crying, irritability, and fussiness after feeding, coupled with signs of lactose intolerance like diarrhea or gas. These formulas provide an alternative nutritional source that may be better tolerated in cases where lactose digestion is compromised.
- Formula Composition
Reduced-lactose formulas are not entirely lactose-free but contain a significantly lower concentration of lactose compared to standard cow’s milk-based formulas. The lactose is often replaced with other carbohydrates, such as glucose polymers or corn syrup solids, to maintain the overall caloric density and nutritional value of the formula.
- Differential Diagnosis
It is imperative to distinguish between lactose intolerance and cow’s milk protein allergy (CMPA), as the management strategies differ. Reduced-lactose formulas may alleviate symptoms related to lactose malabsorption, but they do not address CMPA. Infants with suspected CMPA may require extensively hydrolyzed or amino acid-based formulas for symptom resolution.
Reduced-lactose infant formulas offer a targeted intervention for infants with lactose sensitivity contributing to colic-like symptoms. However, it is crucial to approach their use judiciously, ensuring accurate diagnosis and consideration of alternative etiologies for infant distress, such as CMPA or other gastrointestinal conditions, under the guidance of a healthcare professional.
3. Added Prebiotics
The incorporation of prebiotics into infant formulas formulated for colic management reflects a growing understanding of the gut microbiome’s role in infant health. Prebiotics, non-digestible food ingredients that promote the growth of beneficial bacteria in the gut, are increasingly recognized as a potential strategy to modulate the gut microbiota and alleviate colic symptoms.
- Impact on Gut Microbiota Composition
Prebiotics selectively stimulate the growth and activity of beneficial bacteria such as Bifidobacteria and Lactobacilli in the infant gut. A balanced gut microbiota is associated with improved digestive function, enhanced immune response, and reduced inflammation, potentially mitigating colic symptoms. For instance, studies have shown that infants receiving prebiotic-supplemented formula exhibit a higher abundance of Bifidobacteria, correlating with reduced crying time.
- Modulation of Gut Immune Function
Prebiotics can influence the gut-associated lymphoid tissue (GALT), enhancing immune tolerance and reducing the risk of allergic sensitization. Colic is sometimes associated with heightened gut inflammation or immune dysregulation. Prebiotics may help modulate these immune responses, thereby alleviating symptoms. Certain prebiotics, like galacto-oligosaccharides (GOS) and fructo-oligosaccharides (FOS), have demonstrated the capacity to downregulate pro-inflammatory cytokines in the gut environment.
- Enhanced Bowel Function
Prebiotics promote the production of short-chain fatty acids (SCFAs) by gut bacteria, including acetate, propionate, and butyrate. SCFAs contribute to gut health by providing energy to colonocytes, enhancing gut barrier function, and promoting regular bowel movements. In infants with colic, prebiotics can help soften stools and reduce constipation, potentially alleviating abdominal discomfort. For example, infants fed prebiotics often show improved stool consistency and frequency.
- Synergistic Effect with Probiotics
While prebiotics nourish existing beneficial bacteria, probiotics introduce live beneficial bacteria into the gut. The combination of prebiotics and probiotics, known as synbiotics, can have a synergistic effect in promoting gut health. Some colic formulas include both prebiotics and probiotics to maximize their benefits on gut microbiota composition and function. This combined approach may lead to a more pronounced reduction in colic symptoms compared to prebiotics alone.
The addition of prebiotics to infant formulas represents a targeted approach to modulate the gut microbiota and potentially alleviate colic symptoms. By fostering a beneficial gut environment, prebiotics contribute to improved digestion, enhanced immune function, and reduced inflammation. However, the efficacy of prebiotics in managing colic varies among infants, highlighting the importance of individualized assessment and healthcare professional guidance. Further investigations are required to establish the optimal prebiotic types and dosages for colic management and to identify specific infant subpopulations that may benefit the most from this intervention.
4. Digestive Support
Digestive support constitutes a critical attribute of specialized infant formulas designed for managing colic. The underlying premise is that compromised digestive function contributes significantly to the etiology of colic. Infants experiencing difficulty in digesting or absorbing nutrients may exhibit symptoms such as excessive gas, bloating, abdominal pain, and altered bowel habits, all of which can manifest as inconsolable crying and fussiness characteristic of colic. Therefore, formulas engineered to provide digestive support aim to alleviate these underlying issues, thereby reducing the frequency and intensity of colic episodes. This support typically involves modifications to the formula composition, such as the inclusion of hydrolyzed proteins, reduced lactose content, and/or the addition of prebiotics and probiotics, all intended to ease digestion and promote a healthier gut environment.
The practical significance of digestive support in infant formulas extends beyond merely alleviating colic symptoms. Improved digestion can lead to enhanced nutrient absorption, promoting healthy growth and development. For instance, hydrolyzed proteins, by being pre-digested, reduce the burden on the infant’s digestive system, allowing for more efficient absorption of amino acids essential for tissue building and repair. Similarly, a reduction in lactose can prevent the fermentation of undigested lactose in the colon, minimizing gas production and abdominal discomfort. The addition of prebiotics fosters a favorable gut microbiota composition, further aiding in digestion and nutrient absorption. Real-life examples frequently illustrate the efficacy of these modifications, with parents reporting a noticeable reduction in colic symptoms, improved feeding tolerance, and enhanced overall well-being in their infants following the introduction of digestive support formulas. These observations are often corroborated by healthcare professionals who witness improvements in infant weight gain and general health parameters.
In conclusion, digestive support forms a cornerstone of infant formulas designed to manage colic. By addressing the underlying digestive issues that contribute to colic symptoms, these formulas offer a targeted approach to alleviating infant distress and promoting healthy development. However, it is crucial to recognize that colic is a multifactorial condition, and digestive support formulas may not be universally effective. Therefore, a comprehensive assessment by a healthcare professional is essential to determine the suitability of these formulas and to rule out other potential medical causes of colic. Furthermore, challenges may arise in accurately identifying infants who will benefit most from digestive support formulas, necessitating ongoing research and refined diagnostic approaches.
5. Symptom Alleviation
The primary objective of specialized infant formulas targeting colic centers on symptom alleviation. Colic, characterized by excessive and inconsolable crying in otherwise healthy infants, presents a significant challenge for both infants and caregivers. These formulas are engineered to address the underlying physiological factors contributing to colic, thereby reducing the frequency and intensity of crying episodes. Symptom alleviation is not merely a desirable outcome but a fundamental component of the therapeutic approach embodied by specialized infant formulas.
The practical significance of symptom alleviation is evident in the improved quality of life for both infants and their families. For infants, reduced abdominal discomfort, gas, and irritability translate into increased periods of restful sleep and more positive interactions with caregivers. For parents, the alleviation of colic symptoms reduces stress, anxiety, and feelings of helplessness. Improved infant well-being fosters a more secure and nurturing parent-child bond. Specific examples include formulas with hydrolyzed proteins reducing digestive burden, thus lessening discomfort and crying; reduced lactose formulations alleviating symptoms related to lactose sensitivity; and added prebiotics supporting a healthier gut microbiome, potentially minimizing gas and bloating. Each of these modifications aims to directly address a potential source of infant distress and, consequently, alleviate colic symptoms.
While symptom alleviation is the central aim, it is crucial to recognize that colic is a complex condition with potentially multiple contributing factors. Specialized formulas may not be universally effective, and a comprehensive medical evaluation is essential to rule out other underlying medical conditions. Furthermore, proper feeding techniques, parental support, and environmental factors also play a vital role in managing colic. Symptom alleviation through specialized formulas should, therefore, be viewed as one component of a broader, holistic approach to infant care, always undertaken in consultation with healthcare professionals.
6. Healthcare Guidance
The effective utilization of specialized infant formulas designed to address colic necessitates the integral involvement of healthcare guidance. The selection and implementation of these formulas are not straightforward decisions, and the underlying causes of infant distress are often multifactorial, demanding a comprehensive evaluation by qualified medical professionals. Healthcare guidance provides a structured approach to identifying the potential contributors to colic, differentiating between dietary sensitivities, digestive immaturity, or underlying medical conditions. Without such guidance, parents may inadvertently choose inappropriate formulas or overlook treatable medical issues, potentially delaying appropriate care and prolonging infant distress.
The practical significance of healthcare guidance is exemplified in several clinical scenarios. For instance, an infant presenting with colic symptoms may, in reality, have an undiagnosed cow’s milk protein allergy (CMPA). A healthcare provider can assess the infant’s history, conduct appropriate diagnostic tests, and recommend a suitable extensively hydrolyzed or amino acid-based formula. Similarly, infants with lactose intolerance may benefit from a reduced-lactose formula, but this determination requires careful evaluation to exclude other potential causes of gastrointestinal distress. Moreover, healthcare professionals can provide guidance on proper formula preparation, feeding techniques, and other supportive measures that complement the use of specialized formulas. Furthermore, real-world scenarios may involve situations where colic-like symptoms arise from improper latching, excessive air swallowing during feeding, or other factors that require non-formula related interventions guided by a trained professional.
In summary, healthcare guidance forms an indispensable component of the successful management of colic with specialized infant formulas. It ensures that the formula selection is appropriate for the infant’s specific needs, optimizes feeding practices, and rules out underlying medical conditions. Challenges remain in educating parents about the importance of seeking professional advice and in providing timely access to healthcare services. Linking to the broader theme of infant well-being, healthcare guidance not only addresses colic symptoms but also promotes optimal growth, development, and overall family health.
Frequently Asked Questions About Colic Baby Formula
The following section addresses common inquiries concerning specialized infant formulas intended for the management of colic. These questions and answers aim to provide clarity and guidance based on current understanding and best practices.
Question 1: What is the definition of colic, and how can the presence of colic in an infant be determined?
Colic is defined as excessive and inconsolable crying in an otherwise healthy infant, typically following the “rule of three”: crying for more than three hours per day, more than three days per week, for more than three weeks. Determining the presence of colic requires a comprehensive assessment by a healthcare professional to rule out other potential medical causes of distress.
Question 2: How do specialized infant formulas intended for colic differ from standard infant formulas?
Specialized infant formulas often incorporate modifications such as hydrolyzed proteins, reduced lactose content, and added prebiotics. These modifications aim to improve digestion, reduce gas production, and promote a healthier gut microbiome, potentially alleviating colic symptoms. Standard formulas typically do not contain these specialized components.
Question 3: Is a prescription required to purchase specialized infant formulas designed for colic?
A prescription is not generally required to purchase these formulas. However, consultation with a pediatrician or other healthcare provider is strongly recommended prior to initiating any dietary changes, including the use of specialized formulas.
Question 4: What are the potential side effects associated with the use of specialized infant formulas for colic?
While generally safe, specialized formulas may, in some instances, cause changes in stool consistency or frequency. In rare cases, infants may exhibit allergic reactions to specific ingredients. Close monitoring and consultation with a healthcare professional are essential.
Question 5: How long should a specialized infant formula be used before assessing its effectiveness in alleviating colic symptoms?
A trial period of at least one to two weeks is typically recommended to assess the effectiveness of a specialized formula. However, improvements may be observed sooner. Consistent and careful observation of the infant’s symptoms is critical.
Question 6: Can a specialized infant formula completely eliminate colic in all infants?
No, specialized infant formulas are not universally effective. Colic is a multifactorial condition, and these formulas address only certain potential contributing factors. Other interventions, such as behavioral techniques and parental support, may also be necessary.
In summary, the proper utilization of specialized infant formulas for colic requires careful consideration, healthcare guidance, and a realistic understanding of their potential benefits and limitations.
The following section will provide a comprehensive summary of the key points discussed in this article, reinforcing the importance of informed decision-making in managing infant colic.
Conclusion
This article has thoroughly explored the realm of “colic baby formula,” detailing its composition, mechanisms of action, and role in managing infant distress. Specialized nutrition products designed to address digestive discomfort represent a significant advancement in infant care, offering potential relief to infants and caregivers grappling with persistent crying episodes. Key considerations include hydrolyzed proteins for easier digestion, reduced lactose content to minimize intolerance, and the addition of prebiotics to foster a healthy gut microbiome. However, the content has also emphasized the necessity of healthcare guidance in determining the appropriateness of these products and ruling out underlying medical conditions. Proper selection and usage, combined with supportive care strategies, are crucial for optimizing outcomes.
The utilization of specialized formulas remains an important but not universally effective tool in addressing colic. Continued research into the complex etiology of infant colic and the refinement of nutritional interventions are essential to further improve outcomes. The information presented should empower caregivers to engage in informed discussions with healthcare professionals, facilitating a collaborative approach to addressing the unique needs of each infant, thus promoting optimal health and well-being within the family.