Infant formula is often perceived to satiate infants for longer durations compared to breast milk. This perception stems from differences in composition, specifically higher protein and carbohydrate concentrations, and the slower digestion rate associated with formula. Consequently, some parents believe their infants experience longer periods between feedings when consuming formula. For example, an infant fed breast milk might nurse every two to three hours, while a formula-fed infant might be content for three to four hours before the next feeding.
The significance of this perception lies in its impact on parental feeding choices and schedules. If parents prioritize longer intervals between feedings, they may be more inclined to choose formula over breast milk. Historically, this perception has contributed to the increased use of infant formula, particularly in cultures where parental convenience is highly valued. However, the advantages of breast milk, including its tailored nutritional composition and immunological benefits, should also be carefully considered.
The subsequent sections will delve into the compositional differences between breast milk and infant formula, explore the physiological mechanisms influencing satiety, and examine relevant research on infant feeding behaviors. Furthermore, this exploration will address potential implications for infant health and development, providing a balanced perspective on this critical aspect of infant nutrition.
Considerations Regarding Infant Feeding and Satiety
The following points offer guidance when evaluating infant feeding methods and perceived satiety levels. It is crucial to consult with a healthcare professional for personalized advice.
Tip 1: Evaluate Feeding Cues: Observe an infant’s behavior to determine hunger rather than adhering strictly to a predetermined schedule. Crying is a late indicator of hunger; earlier cues include rooting, sucking on hands, and increased alertness.
Tip 2: Recognize Individual Variation: Infants exhibit diverse metabolic rates and growth patterns. One infant may require more frequent feedings, while another may be content with longer intervals, irrespective of feeding method.
Tip 3: Understand Formula Composition: Different formulas contain varying ratios of proteins, carbohydrates, and fats. Higher protein content, for example, may contribute to a feeling of fullness, but the suitability of each formula should be discussed with a pediatrician.
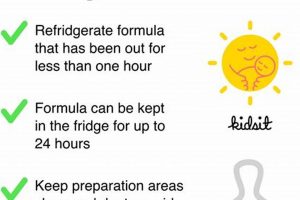
Tip 4: Be Mindful of Feeding Volume: Formula-fed infants may consume larger volumes at each feeding, contributing to a sense of fullness. Ensure appropriate bottle size and pace the feeding to allow the infant to recognize satiety cues.
Tip 5: Acknowledge Digestive Differences: Breast milk is generally digested more rapidly than formula. This quicker digestion rate does not necessarily equate to inadequate satiation; rather, it reflects the inherent properties of breast milk.
Tip 6: Consult Healthcare Professionals: If concerns arise regarding an infant’s feeding patterns, growth, or perceived hunger levels, seek guidance from a pediatrician or lactation consultant. These professionals can provide tailored recommendations based on the infant’s individual needs.
Tip 7: Observe Stooling Patterns: Changes in stool frequency or consistency may indicate issues with formula tolerance or digestion. Report any significant alterations to a healthcare provider.
These considerations highlight the complexity of infant feeding and satiety. A holistic approach, encompassing observation, professional guidance, and an understanding of individual infant needs, is paramount. This understanding prepares the way for a concluding summary of the key insights explored within this article.
1. Compositional differences matter
The distinct compositions of breast milk and infant formula play a crucial role in the perceived duration of satiety experienced by infants. These differences, particularly in macronutrient ratios and the presence of bioactive components, influence digestion rates and hormonal responses, thereby affecting the intervals between feedings. Understanding these compositional nuances is essential when addressing parental concerns regarding infant fullness and feeding schedules.
- Protein Ratio
Infant formulas generally contain higher protein concentrations than breast milk. This elevated protein level can lead to slower gastric emptying, prolonging the feeling of fullness. For example, casein-dominant formulas, which digest more slowly than whey-dominant formulas, may result in longer intervals between feedings compared to breast milk, which is primarily whey-based. However, the long-term effects of high protein intake on infant metabolism are a subject of ongoing research.
- Carbohydrate Source
Lactose is the primary carbohydrate in both breast milk and most infant formulas. However, some formulas utilize alternative carbohydrate sources such as corn syrup solids or sucrose. These different carbohydrate types may affect blood glucose levels and insulin release, influencing appetite regulation. Breast milk’s lactose is digested more readily than certain other carbohydrates, potentially leading to faster glucose absorption and subsequent decline, thus contributing to more frequent feeding cues.
- Fat Composition
Breast milk contains a diverse array of fats, including long-chain polyunsaturated fatty acids (LCPUFAs) like DHA and ARA, which are essential for brain development. While formulas are increasingly fortified with these fatty acids, the overall fat composition and digestibility can differ. Breast milk’s fats are typically more easily absorbed due to the presence of lipase, an enzyme that aids in fat digestion. This enhanced digestibility might lead to quicker nutrient absorption and a potentially shorter duration of satiety.
- Bioactive Components
Breast milk contains numerous bioactive components, including hormones, enzymes, and immunoglobulins, which contribute to its unique properties. These components influence gut microbiota composition, immune system development, and appetite regulation. For instance, leptin, a hormone involved in satiety signaling, is present in breast milk but not in standard infant formulas. The absence of such bioactive factors in formula may affect the infant’s ability to self-regulate appetite and perceive fullness in the same way as a breastfed infant.
In conclusion, the compositional distinctions between breast milk and infant formula exert a considerable influence on infant satiety. While higher protein levels in formula may prolong the feeling of fullness, the unique fat composition and bioactive components of breast milk contribute to its distinct digestive properties and potential for more frequent feeding cues. A comprehensive understanding of these factors is paramount for healthcare professionals and parents seeking to make informed decisions regarding infant feeding practices, while considering the nuances of “does formula make babies fuller”.
2. Digestion rate variations
The rate at which an infant digests breast milk or formula significantly impacts the perception of fullness and the frequency of feeding cues. Variations in digestion rates are primarily attributed to the differing compositions of breast milk and formula, affecting gastric emptying times and nutrient absorption. These differences contribute to the debate surrounding whether formula induces longer periods of satiety in infants.
- Protein Structure and Digestion
Breast milk contains a higher proportion of whey protein, which is more easily and quickly digested than casein, the predominant protein in many infant formulas. Casein forms a curd in the stomach, leading to slower gastric emptying and a prolonged feeling of fullness. For instance, an infant fed a casein-dominant formula may experience a slower release of amino acids into the bloodstream compared to an infant fed breast milk, potentially delaying hunger cues. The slower digestion of casein thus may correlate to extended periods between feedings.
- Fat Content and Absorption Efficiency
While the overall fat content can be similar between breast milk and formula, the structure and digestibility of fats differ. Breast milk contains lipase, an enzyme that aids in fat digestion, enhancing absorption efficiency. Formulas, lacking this enzyme, may result in slower fat digestion. The slower absorption of fats in formula could contribute to a longer feeling of satiety as the digestive system processes these nutrients over an extended period. Example is absorption efficiency is vital process that correlate of “does formula make babies fuller”.
- Carbohydrate Complexity and Breakdown
Lactose, the primary carbohydrate in both breast milk and most formulas, is readily digested by infants. However, some formulas incorporate more complex carbohydrates like corn syrup solids, which may require more time for enzymatic breakdown. This slower breakdown process can affect the rate at which glucose is released into the bloodstream, influencing satiety signals. An infant consuming a formula with complex carbohydrates may experience a more gradual rise in blood glucose, potentially contributing to a longer feeling of fullness.
- Gastric Emptying Time Differences
The cumulative effect of protein structure, fat content, and carbohydrate complexity influences gastric emptying timethe rate at which food empties from the stomach into the small intestine. Breast milk generally empties from the stomach more quickly than formula due to its easily digestible components. Studies have shown that formula-fed infants may have a slower gastric emptying rate, contributing to the perception that they feel fuller for a longer duration. Example is that formula have longer gastric emptying rate that lead to longer duration.
In conclusion, the variations in digestion rates between breast milk and formula stem from fundamental differences in their composition, affecting protein breakdown, fat absorption, carbohydrate complexity, and overall gastric emptying time. These factors collectively influence the perception of fullness and contribute to the discussion surrounding whether formula provides a longer-lasting sense of satiety compared to breast milk. These dynamics ultimately impact parental decisions and infant feeding schedules.
3. Protein content impact
The protein content in infant formula significantly influences satiety and thus contributes to the perception of whether formula makes babies feel fuller. Higher protein concentrations, commonly found in infant formula compared to breast milk, slow gastric emptying. This prolonged digestion leads to a more sustained release of amino acids into the bloodstream, which can suppress appetite hormones. Consequently, infants consuming higher-protein formulas may exhibit longer intervals between feedings. An example is a comparison of whey-dominant versus casein-dominant formulas. Casein, being a slower-digesting protein, often results in a more extended sense of fullness. The understanding of protein content impact is crucial for parents and healthcare professionals when choosing an appropriate feeding method.
The practical application of this understanding lies in tailoring infant feeding strategies. If a parent prioritizes less frequent feedings, a formula with a higher protein content might seem advantageous. However, this choice should be balanced against potential long-term effects of high protein intake on infant metabolic development. Furthermore, the source of protein and its digestibility are important considerations. Hydrolyzed protein formulas, for instance, may be more easily digested despite a higher protein content, potentially affecting satiety differently. It is essential to acknowledge that not all proteins are created equal in the context of infant digestion and metabolism.
In summary, the protein content of infant formula affects the duration of satiety experienced by infants. The impact is multi-faceted, involving gastric emptying, hormonal regulation, and protein digestibility. While higher protein content may extend the interval between feedings, potential long-term health implications and the importance of matching protein source to infant needs require careful consideration. This exploration highlights the complex interplay between protein composition, infant physiology, and parental feeding choices in infant nutrition.
4. Caloric density variance
Caloric density, defined as the number of calories per unit volume, is a significant factor influencing infant satiety and the perception that formula feeding results in a greater sense of fullness. Infant formulas generally exhibit a more consistent caloric density compared to breast milk, which can vary based on maternal diet, time of day, and stage of lactation. This consistency in caloric density may contribute to more predictable feeding intervals and a prolonged feeling of satiety in formula-fed infants. For instance, a standard infant formula provides approximately 20 calories per ounce, while breast milk’s caloric density can fluctuate, potentially leading to variations in the infant’s satiety levels. This consistency can give parents the impression that formula makes babies fuller due to the predictable nature of the satiety response.
The impact of caloric density variance is particularly relevant when considering infant weight gain and growth patterns. Higher caloric density, as found in some specialized formulas, can be intentionally used to promote weight gain in infants who are failing to thrive. However, consistent overfeeding with high-caloric-density formulas can potentially lead to excessive weight gain and may increase the risk of obesity later in life. Conversely, lower caloric density in certain breast milk samples may result in more frequent feeding cues, reflecting the infant’s need to consume more volume to meet their energy requirements. Therefore, understanding and managing caloric density is crucial for optimizing infant nutrition and promoting healthy growth trajectories. An example of mismanagement may result in weight gain issues.
In conclusion, caloric density variance plays a critical role in determining infant satiety and influencing feeding behaviors. The consistent caloric density of infant formula, compared to the variability in breast milk, can contribute to the perception that formula feeding makes babies feel fuller for longer periods. However, awareness of these differences is essential for informed decision-making regarding infant feeding practices. The long-term implications of consistent high or low caloric density underscore the need for careful monitoring of infant growth and adjustment of feeding strategies as needed. Such informed practices will enhance the overall health and development of infants.
5. Individual metabolic rates
Individual metabolic rates introduce a significant variable in the perception of fullness after feeding, irrespective of whether an infant consumes breast milk or formula. These rates, which dictate how efficiently an infant processes nutrients and expends energy, can modify the duration between feedings and influence the perceived satiety derived from each feeding. Discrepancies in metabolic activity can lead to varied conclusions regarding the satiating effect of different feeding methods.
- Basal Metabolic Rate (BMR) Influence
BMR, representing the energy expended at rest, varies significantly among infants. Infants with higher BMRs require more frequent feedings to meet their energy demands, regardless of the feeding method. A formula-fed infant with a high BMR might exhibit hunger cues sooner than a breastfed infant with a lower BMR, challenging the assumption that formula inherently leads to longer satiety. This variability can influence the perception of whether formula is truly more satiating.
- Activity Level Considerations
An infant’s activity level significantly affects energy expenditure and, consequently, feeding frequency. More active infants utilize energy at a faster rate, requiring more frequent replenishment through feedings. A highly active formula-fed infant might need to be fed as frequently as a less active breastfed infant. Thus, activity level can override any inherent differences in satiety between breast milk and formula, complicating the determination of “does formula make babies fuller.”
- Thermic Effect of Food (TEF) Impact
TEF, the energy expended to digest, absorb, and metabolize nutrients, varies depending on the composition of the food. While formula and breast milk differ in their macronutrient profiles, the overall TEF impact may be relatively similar. However, subtle differences in protein and fat digestion could influence TEF, potentially affecting satiety. An infant with a higher TEF might experience a slightly longer period of satiety, but this effect is often overshadowed by the more significant influence of BMR and activity level.
- Hormonal Regulation of Metabolism
Hormones such as thyroid hormones and growth hormone play a crucial role in regulating metabolic rate. Variations in hormone levels can significantly affect energy expenditure and appetite. Infants with hormonal imbalances may exhibit altered feeding patterns and satiety cues, regardless of whether they are formula-fed or breastfed. These hormonal influences introduce another layer of complexity in understanding whether formula truly provides longer-lasting satiety, independent of individual metabolic characteristics.
In conclusion, individual metabolic rates introduce substantial variability in infant feeding patterns and satiety perceptions. While formula composition and caloric density play a role, BMR, activity level, TEF, and hormonal influences collectively determine an infant’s energy requirements and feeding frequency. These factors underscore the complexity in determining whether formula inherently makes babies fuller, highlighting the importance of considering individual metabolic characteristics alongside feeding method when evaluating infant satiety.
6. Feeding volume control
Feeding volume control plays a critical role in the perception of satiety and directly influences whether formula is perceived to make babies fuller. The ability to regulate and standardize the amount of formula consumed at each feeding, in contrast to the more variable intake during breastfeeding, affects the duration between feedings and the overall impression of fullness. This controlled aspect is central to understanding infant feeding behaviors and parental perceptions.
- Standardized Measurement and Intake
Formula feeding allows for precise measurement and delivery of a specified volume at each feeding. This standardization provides predictability in caloric intake, potentially leading to more consistent satiety signals. For example, a parent can consistently offer a 4-ounce bottle, delivering a known quantity of calories. This contrasts with breastfeeding, where the exact volume ingested is often unknown, leading to variations in satiety and feeding frequency. The standardized intake facilitates parental perception that formula provides a more reliable sense of fullness.
- Parental Perception and Control
Parents often perceive formula feeding as offering greater control over their infant’s intake. This control can lead to deliberate adjustments in feeding volume based on perceived hunger cues or weight gain goals. For instance, a parent might increase the volume offered at each feeding to promote weight gain or reduce the frequency of feedings. This active management of volume contributes to the belief that formula allows for greater regulation of an infant’s satiety. However, such control can also lead to overfeeding if not guided by infant cues.
- Bottle-Feeding Dynamics and Flow Rate
The mechanics of bottle-feeding can influence the pace and volume of intake. Bottles with faster flow rates may encourage infants to consume larger volumes more quickly, potentially leading to a greater sense of fullness. Conversely, slower flow rates may result in smaller intakes and more frequent feedings. The choice of bottle and nipple type can thus affect the perceived satiating effect of formula, impacting the parental perspective on whether formula “makes babies fuller” due to the mechanical aspects of feeding.
- Overfeeding Risks and Satiety Cues
While controlled feeding volume offers advantages, it also presents the risk of overfeeding. Parents may encourage infants to finish bottles even when they exhibit signs of satiety, overriding the infant’s natural hunger and fullness cues. This can lead to chronic overconsumption and a distorted perception of appropriate feeding volumes. An example is pressuring infant to finish bottle even when infant is signalling fullness. As a result, while formula feeding enables volume control, it is crucial to remain attuned to the infant’s individual needs and responses to avoid disrupting natural satiety mechanisms.
In conclusion, feeding volume control significantly influences the perception that formula makes babies fuller. The ability to standardize intake, parental control over volume, bottle-feeding dynamics, and the potential for overfeeding all contribute to this perception. While formula feeding provides tools for managing feeding volumes, it is crucial to balance this control with attentiveness to infant cues and a commitment to promoting healthy feeding habits. This informed approach ensures appropriate infant nutrition and prevents the distortion of natural satiety mechanisms.
7. Parental perception biases
Parental perception biases significantly influence the belief that formula makes babies fuller. These biases, shaped by cultural norms, marketing influences, and personal experiences, often lead parents to interpret infant behaviors through a lens that favors formula feeding. For example, a parent may attribute a longer sleep duration to the satiating effect of formula, overlooking other factors such as infant temperament or sleep patterns. These biases create a self-reinforcing cycle where perceived benefits are amplified, solidifying the conviction that formula provides superior satiety. The importance of recognizing these biases lies in promoting informed, evidence-based decision-making in infant feeding practices, as they can overshadow objective assessments of infant needs and behaviors.
The impact of marketing is a primary driver of these biases. Formula manufacturers often emphasize the convenience and satiety associated with their products, creating associations in parents’ minds. Furthermore, societal expectations regarding infant sleep schedules and parental convenience can reinforce the perception that longer intervals between feedings are desirable. Practical implications include the potential for overfeeding formula-fed infants if parents prioritize scheduled feedings over responsive feeding based on hunger cues. Consequently, infants may be encouraged to consume larger volumes than needed, leading to potential weight gain issues. Therefore, understanding the underlying biases that affect perceptions of fullness becomes critical in guiding feeding practices. An example of social expectation affect perception is desire for infant to sleep for long period.
In summary, parental perception biases play a substantial role in shaping beliefs about formula’s impact on infant satiety. Cultural influences, marketing strategies, and individual experiences contribute to these biases, affecting feeding decisions and potentially impacting infant health. Recognizing and mitigating these biases through education and a focus on responsive feeding can promote healthier infant feeding practices. Addressing these biases allows for a more objective evaluation of infant needs, fostering informed choices that support optimal infant development.
Frequently Asked Questions
The following addresses common inquiries regarding infant formula and its impact on satiety levels in infants.
Question 1: Does infant formula genuinely keep babies fuller for extended durations compared to breast milk?
The perception of prolonged satiety with infant formula stems from its composition. Infant formula typically contains higher protein and, in some cases, more complex carbohydrate concentrations than breast milk. These components digest more slowly, potentially leading to longer intervals between feedings.
Question 2: How do formula ingredients influence an infants sense of fullness?
Protein, specifically casein found in certain formulas, digests more slowly than the whey protein predominant in breast milk. This delayed digestion can contribute to a prolonged feeling of fullness. Additionally, the inclusion of complex carbohydrates or specific fat types can affect digestion rates and satiety signals.
Question 3: Is increased satiety, from formula, beneficial for all infants?
Increased satiety, leading to longer intervals between feedings, may not be universally beneficial. Breast milk’s composition adapts to the infant’s evolving needs, offering tailored nutrition. Formula, while providing essential nutrients, lacks this adaptability. Furthermore, prolonged intervals may not align with an infant’s individual metabolic rate or growth spurts.
Question 4: Does the consistent caloric density of formula impact satiety differently compared to breast milk?
Infant formula maintains a relatively consistent caloric density, offering predictable energy intake. Breast milk caloric density varies based on factors such as maternal diet and time of day. This consistent caloric density in formula may contribute to more predictable satiety patterns, whereas breast milk feedings adapt to the infant’s varying needs.
Question 5: Could parental perceptions influence the belief that formula-fed infants are fuller?
Parental perceptions, often shaped by societal norms, marketing, and personal experiences, may influence how they interpret infant feeding behaviors. The desire for longer sleep intervals or less frequent feedings could lead parents to perceive formula as providing superior satiety, even if other factors are at play.
Question 6: What are the potential risks associated with prioritizing fullness over responsive feeding?
Prioritizing prolonged fullness over responsive feeding, which involves feeding based on infant hunger cues, may disrupt the infant’s natural ability to self-regulate intake. This can lead to overfeeding, potential weight gain issues, and a reduced capacity to recognize internal satiety signals over time. It is crucial to feed infant based on their cues and not some measurement result from formula.
These responses address key concerns surrounding infant formula and satiety. However, individual infant needs and circumstances vary. Consulting with healthcare professionals ensures informed, appropriate feeding strategies.
Subsequent content will provide a concluding summary of the key insights.
Conclusion
The exploration of whether “does formula make babies fuller” reveals a nuanced interplay of physiological and perceptual factors. While compositional differences between infant formula and breast milk, such as higher protein content and consistent caloric density, can contribute to prolonged digestion and potentially longer intervals between feedings, individual metabolic rates, feeding volumes, and parental perception biases also exert significant influence. These elements challenge simplistic conclusions about formula’s inherent superiority in promoting satiety.
Ultimately, the decision regarding infant feeding should prioritize the infant’s individual needs and hunger cues, fostering responsive feeding practices that support healthy growth and development. Future research is needed to further elucidate the long-term metabolic and behavioral impacts of different feeding methods, ensuring that parental choices are guided by the most robust scientific evidence. A collaborative dialogue between healthcare professionals and parents is crucial to navigate the complexities of infant nutrition effectively.