Administering formula to infants directly from the refrigerator raises concerns about potential digestive discomfort and reluctance to feed. The primary question revolves around whether the temperature of the prepared formula impacts a baby’s well-being and feeding experience. Infants generally prefer milk that is either body temperature or slightly warmer, mirroring the temperature of breast milk.
The significance of warming formula stems from facilitating easier digestion and mimicking the natural feeding process. Historically, warming practices have aimed to provide comfort and encourage optimal nutrient absorption. While not inherently dangerous, cold formula can lead to fussiness, gas, and a less enjoyable feeding experience for the infant. Consistent administration of warmed formula can contribute to more comfortable and predictable feeding routines.
Therefore, subsequent sections will address the physiological impact of cold formula, recommended warming techniques, and potential alternatives to ensure safe and comfortable feeding practices for infants. We will also discuss scenarios where cold formula might be unavoidable and how to mitigate any adverse effects. The following discussion will provide a comprehensive understanding of appropriate formula preparation and delivery.
Considerations Regarding Formula Temperature
The following tips address optimal formula preparation and delivery to minimize potential issues related to temperature.
Tip 1: Prioritize Warming. When feasible, warming formula to body temperature (approximately 98.6F or 37C) is advisable. This can be achieved using a bottle warmer or by placing the bottle in a container of warm water.
Tip 2: Test the Temperature. Before feeding, always test the formula’s temperature on the inner wrist. It should feel lukewarm, not hot.
Tip 3: Avoid Microwaving. Microwaving formula is not recommended due to uneven heating, which can create hot spots that could burn the infant.
Tip 4: Observe Infant’s Reactions. Pay close attention to the infant’s cues during feeding. Signs of discomfort, such as fussiness or refusal to feed, may indicate the formula is too cold.
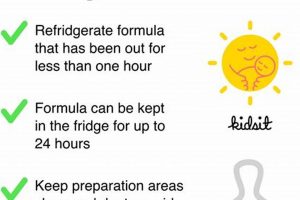
Tip 5: Prepare Formula as Needed. Preparing formula in advance and storing it in the refrigerator is acceptable, but it should be warmed before feeding. Discard any unused formula after feeding.
Tip 6: Room Temperature as an Alternative. If warming is not possible, formula at room temperature is preferable to cold formula. Allowing prepared formula to sit at room temperature for a short period before feeding can mitigate some temperature-related issues.
Tip 7: Consistency is Key. Maintain a consistent feeding temperature to minimize digestive upset and establish predictable feeding routines.
Adhering to these guidelines can help ensure a comfortable and positive feeding experience for the infant, minimizing potential adverse effects related to formula temperature.
The next section will delve into the rare circumstances when cold formula is necessary and how to deal with it.
1. Digestive discomfort
The administration of cold formula may induce digestive discomfort in infants due to the temperature differential between the formula and the infant’s internal body temperature. This temperature variation can lead to physiological responses within the infant’s digestive system, potentially causing gastrointestinal distress. Specifically, cold liquids can slow down the digestive process, increasing the likelihood of gas formation and abdominal cramping. The immature digestive systems of infants are often more sensitive to such temperature fluctuations compared to older children or adults, making them more susceptible to these discomforts.
Real-world examples include instances where infants fed cold formula exhibit increased fussiness, crying, or arching of the back after feeding, indicative of abdominal pain. Healthcare providers often advise parents to warm formula to body temperature or slightly above to mitigate these issues. This recommendation stems from the understanding that warmer formula is more easily processed by the infant’s digestive system, reducing the likelihood of digestive upset. The practical significance of this understanding lies in the ability to alleviate infant distress and promote more comfortable feeding experiences.
In summary, digestive discomfort serves as a crucial indicator of the potential negative impact of cold formula on infants. Recognizing and addressing this discomfort through appropriate formula warming techniques can lead to improved infant comfort and feeding tolerance. Overlooking this aspect may result in prolonged periods of fussiness, feeding difficulties, and potential growth issues. Addressing cold formula’s impact on digestion helps ensure optimal nutrient absorption.
2. Feeding reluctance
Feeding reluctance in infants, particularly when associated with formula feeding, often presents as a significant challenge for caregivers. This aversion to feeding can stem from various factors, with formula temperature being a notable contributor. The issue warrants careful consideration to ensure adequate nutrition and promote healthy growth.
- Sensory Aversion
Infants possess heightened sensory perceptions, making them acutely sensitive to stimuli such as temperature. Cold formula can create an unpleasant sensory experience, leading to an immediate rejection of the bottle. This aversion is not merely a matter of preference but can trigger a physiological response, such as gagging or spitting up, further reinforcing the negative association with feeding. For instance, an infant repeatedly offered cold formula may develop a conditioned aversion, anticipating the unpleasant sensation and actively resisting feeding attempts. This can lead to decreased caloric intake and potential nutritional deficiencies.
- Gastrointestinal Discomfort Association
Beyond the initial sensory experience, cold formula can induce gastrointestinal discomfort, exacerbating feeding reluctance. The digestive system of an infant is still developing and may struggle to process cold liquids efficiently. This can result in gas, bloating, and abdominal cramping, creating a painful experience associated with feeding. An infant experiencing such discomfort may learn to associate the bottle with pain, actively avoiding feeding sessions to prevent the recurrence of these symptoms. This avoidance behavior can be difficult to overcome and may require intervention from healthcare professionals.
- Disruption of Feeding Patterns
Consistent administration of cold formula can disrupt established feeding patterns. Infants thrive on routine and predictability, including consistent feeding temperatures. Fluctuations in formula temperature can confuse the infant, making it difficult to anticipate and prepare for feeding. This inconsistency can lead to frustration and anxiety during feeding times, resulting in a reluctance to engage in the feeding process. Parents who consistently offer warmed formula often find that their infants readily accept feedings, establishing a positive association with the bottle and promoting more predictable feeding schedules.
- Mimicking Breast Milk Temperature
The temperature of breast milk is naturally close to the mother’s body temperature. Infants are biologically programmed to expect this warmth during feeding. Cold formula deviates significantly from this expectation, potentially disrupting the infant’s innate feeding instincts. Mimicking the warmth of breast milk by warming formula can help to align with these natural expectations, making the feeding process more comforting and acceptable to the infant. This alignment can reduce feeding reluctance and promote a more positive feeding experience, fostering a stronger bond between caregiver and infant.
In conclusion, feeding reluctance, when viewed in the context of temperature, highlights the critical importance of carefully considering formula preparation methods. The complex interplay between sensory perception, gastrointestinal function, and behavioral conditioning underscores the potential for cold formula to negatively impact an infant’s willingness to feed. Addressing this issue through consistent warming practices can significantly improve feeding outcomes, ensuring adequate nutrition and promoting overall well-being.
3. Nutrient absorption
The relationship between nutrient absorption and the temperature of infant formula centers on physiological processes within the infant’s digestive system. Cold formula can potentially impede optimal nutrient absorption due to several factors. The body expends energy to warm the ingested liquid, diverting resources from digestive functions. Additionally, the reduced temperature may slow enzymatic activity responsible for breaking down complex nutrients into absorbable forms. Consequently, the transit time of the formula through the digestive tract may be altered, diminishing the opportunity for complete nutrient uptake. For example, essential fats, crucial for brain development and energy provision, might not be fully emulsified and absorbed if the formula is ingested cold, leading to suboptimal utilization of these nutrients.
Further implications arise from the potential for gastrointestinal distress caused by cold formula. Infants experiencing discomfort, such as gas or abdominal cramping, may exhibit reduced appetite and feeding reluctance. This can lead to decreased overall formula consumption, indirectly impacting nutrient intake. Furthermore, gastrointestinal inflammation, though not directly caused by cold formula alone, can compromise the integrity of the intestinal lining, hindering nutrient absorption. The practical application of this understanding lies in recognizing the importance of warming formula to a temperature that facilitates efficient digestion and absorption. Consistent application of warmed formula contributes to optimal growth and development by ensuring that the infant receives the full nutritional benefit of the formula.
In summary, the issue extends beyond mere preference, highlighting a potential compromise in the efficiency of nutrient absorption. While not directly causing malnutrition, cold formula can act as a contributing factor to suboptimal nutrient utilization, particularly in infants with sensitive digestive systems. Therefore, healthcare recommendations generally emphasize warming formula to promote enhanced digestion and nutrient uptake, supporting the broader goal of ensuring adequate nutrition for optimal infant health. Acknowledging challenges and implementing warming strategies reinforces the commitment to providing infants with the best possible conditions for growth and development.
4. Body temperature mimicry
The concept of body temperature mimicry plays a pivotal role in infant feeding, particularly concerning the delivery of formula. Replicating the warmth of breast milk through appropriately heated formula aims to facilitate optimal digestion, comfort, and acceptance by the infant.
- Physiological Alignment
Infants possess a physiological expectation of warmth during feeding, mirroring the temperature of breast milk, typically around 98.6F (37C). Formula presented at significantly lower temperatures deviates from this expectation, potentially triggering physiological stress. The body must expend energy to warm the ingested liquid, diverting resources from other critical functions, such as digestion and nutrient absorption. By delivering formula at a temperature close to body temperature, this energy expenditure is minimized, allowing the infant’s system to focus on efficient digestion and nutrient uptake.
- Digestive Enzyme Activity
Enzymatic activity within the digestive system is temperature-dependent. Enzymes responsible for breaking down complex carbohydrates, proteins, and fats function optimally within a narrow temperature range, approximating body temperature. Cold formula can reduce the efficiency of these enzymes, potentially hindering the breakdown of nutrients into absorbable forms. This incomplete digestion may lead to gastrointestinal discomfort, such as gas or bloating, and may also decrease the overall bioavailability of essential nutrients. The practical significance lies in ensuring that formula is warmed appropriately to support optimal enzymatic function and efficient nutrient digestion.
- Comfort and Acceptance
The tactile and sensory experience of feeding contributes significantly to an infant’s overall acceptance of formula. Cold formula can create an unpleasant sensation in the mouth and esophagus, leading to feeding reluctance or refusal. By contrast, formula that is warmed to body temperature provides a comforting and familiar sensation, promoting a more relaxed and positive feeding experience. This improved comfort can encourage the infant to consume a sufficient volume of formula, ensuring adequate caloric intake and supporting healthy growth and development. The sensory dimension of temperature therefore plays a crucial role in feeding success.
- Regulation of Gastric Emptying
The rate of gastric emptying, the process by which food moves from the stomach into the small intestine, is influenced by the temperature of ingested substances. Cold liquids can slow gastric emptying, potentially leading to feelings of fullness and discomfort. This delayed emptying may also reduce the frequency of feedings, impacting overall nutrient intake. By warming formula to body temperature, gastric emptying can proceed at a more natural and efficient rate, promoting a more regular feeding schedule and optimizing nutrient delivery to the small intestine for absorption. The dynamic between temperature and gastric motility underscores the physiological rationale for temperature regulation.
These facets illustrate the intricate connections between body temperature mimicry and infant formula feeding. Administering cold formula deviates from the infant’s physiological expectations, potentially hindering digestion, nutrient absorption, and overall comfort. By adhering to recommended warming practices, caregivers can promote a more positive and efficient feeding experience, supporting optimal growth and development.
5. Gastrointestinal issues
The relationship between cold formula and gastrointestinal distress in infants presents a significant concern for caregivers and pediatric healthcare providers. The immature digestive systems of infants are particularly susceptible to external factors such as temperature, making the administration of cold formula a potential contributor to various gastrointestinal issues. Understanding these issues and their underlying mechanisms is crucial for promoting infant comfort and well-being.
- Increased Gas Production
The ingestion of cold formula can slow down the digestive process, leading to increased fermentation of undigested lactose and other carbohydrates in the colon. This fermentation results in the production of excess gas, causing abdominal distension, discomfort, and increased crying. Infants with immature digestive systems are less efficient at processing lactose, making them more prone to gas production when consuming cold formula. For instance, an infant experiencing frequent episodes of inconsolable crying after feeding may be exhibiting symptoms of gas-related abdominal pain linked to cold formula consumption.
- Exacerbation of Colic Symptoms
Colic, characterized by excessive and unexplained crying in otherwise healthy infants, can be exacerbated by gastrointestinal discomfort. Cold formula may contribute to colic symptoms by increasing gas production, causing abdominal cramping, and disrupting normal digestive processes. Infants with colic often exhibit heightened sensitivity to environmental stimuli, and the discomfort associated with cold formula can further intensify their distress. Empirical observations indicate that switching to warmed formula can sometimes alleviate colic symptoms, suggesting a direct link between formula temperature and gastrointestinal irritability.
- Increased Risk of Regurgitation and Vomiting
The administration of cold formula can potentially disrupt the normal function of the lower esophageal sphincter (LES), the muscle that prevents stomach contents from refluxing back into the esophagus. Cold temperatures can weaken LES tone, increasing the likelihood of regurgitation or vomiting. Infants with gastroesophageal reflux (GER) may experience worsened symptoms when fed cold formula. Healthcare professionals often recommend warming formula to reduce the risk of regurgitation, thereby minimizing discomfort and preventing potential complications such as esophagitis.
- Altered Gut Motility
Cold formula can affect gut motility, the rhythmic contractions of the digestive tract that propel food through the system. Cold temperatures can slow down these contractions, leading to delayed gastric emptying and prolonged transit time. This altered motility can contribute to constipation or, conversely, to diarrhea, depending on the individual infant’s physiological response. Disruptions in gut motility can also interfere with nutrient absorption, potentially leading to nutritional deficiencies over time. Careful monitoring of stool patterns and consistency is essential for identifying and addressing any motility-related issues linked to formula temperature.
In conclusion, various gastrointestinal issues underscore the significance of adhering to recommended formula preparation guidelines. The impact of cold formula on gas production, colic symptoms, regurgitation risk, and gut motility highlights the importance of warming formula to promote infant comfort and digestive health. Recognizing the potential for these complications and implementing appropriate warming strategies can contribute significantly to improving infant well-being.
Frequently Asked Questions About Infant Formula Temperature
The following section addresses common inquiries regarding the impact of formula temperature on infant health and feeding practices.
Question 1: Can cold formula directly harm an infant?
While cold formula is unlikely to cause direct, immediate harm, it may contribute to digestive discomfort, feeding reluctance, and potentially suboptimal nutrient absorption in some infants. The degree of impact can vary based on individual sensitivity and overall health.
Question 2: Is warming formula always necessary?
Warming formula to approximately body temperature (around 98.6F or 37C) is generally recommended to promote comfort and facilitate digestion. However, if warming is not feasible, formula at room temperature is preferable to administering it cold. Consistent feeding practices are also an important key.
Question 3: What is the safest method for warming infant formula?
The safest method involves using a bottle warmer or placing the bottle in a container of warm water. Microwaving is not recommended due to the risk of uneven heating and potential burns. The temperature of the warmed formula should always be tested on the inner wrist before feeding.
Question 4: Are there any benefits to administering cold formula?
There are no known benefits to administering cold formula. The prevailing recommendations emphasize warming to mimic breast milk temperature and facilitate optimal digestion.
Question 5: How does cold formula affect nutrient absorption?
Cold formula may potentially impede nutrient absorption by slowing down digestive processes and reducing the efficiency of digestive enzymes. This can lead to suboptimal utilization of essential nutrients, particularly in infants with sensitive digestive systems.
Question 6: What are the signs of digestive discomfort related to cold formula?
Signs of digestive discomfort may include increased fussiness, crying, gas, abdominal distension, and feeding refusal. Observation of these symptoms warrants consideration of warming the formula before subsequent feedings.
In summary, while not inherently dangerous, cold formula can pose potential challenges to infant comfort and digestion. The best practice involves warming formula to approximate body temperature, ensuring a more pleasant and efficient feeding experience.
The next section will focus on strategies for transitioning an infant accustomed to cold formula to warmed formula, minimizing potential feeding disruptions.
Is Cold Formula Bad for Babies
This exploration has rigorously examined the question of “is cold formula bad for babies,” revealing potential implications for infant comfort, digestion, and nutrient absorption. The findings indicate that while cold formula is not acutely dangerous, its administration may contribute to digestive discomfort, feeding reluctance, and reduced enzymatic efficiency, potentially impacting optimal nutrient uptake. The consensus among healthcare professionals favors warming formula to approximate body temperature, mirroring the natural warmth of breast milk and facilitating efficient digestion.
Given the potential adverse effects, caregivers are encouraged to prioritize warming formula whenever feasible, adhering to established safety guidelines to prevent burns. Consistent attention to feeding temperature and close observation of infant cues can promote a more positive and nutritionally beneficial feeding experience. Future research should further investigate the long-term implications of formula temperature on infant gut health and overall development, informing evidence-based feeding practices for optimal infant well-being.